The genitals are essential parts of the body, and their functions cannot be overemphasized, and various structures such as tissues, vessels, and glands are found around them.
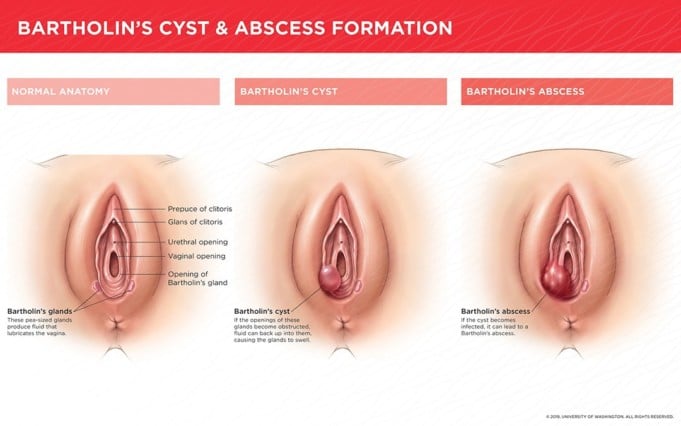
One of these vital glands found in the vagina is the Bartholin’s gland. A Bartholin’s gland is a tiny gland found resting on each side of the vaginal lips (labia) near the vagina opening. If we compare the vagina to a clock’s face, the Bartholin’s gland can be located at around 4 and 8 o’clock.
The glands are named after Danish anatomist Caspar Bartholin the Younger (1655-1738). Caspar made the first detailed study of the gland’s physiology and anatomy in humans.
Bartholin’s glands are usually not visible to the eyes, and its function is to secrete a type of fluid through openings that lubricate the vagina during intense friction, such as during sexual intercourse, to prevent a tear of the vaginal labia. The fluid usually is colorless and odorless and has a high level of viscosity.
Bartholin’s cysts or Bartholin’s duct cysts are sometimes called benign tumors that occur when one or both of the glands swell up due to the accumulation of fluid in the gland.
The fluid accumulation may be due to a flap of skin growing over the opening of one of the glands; when this happens, it causes backing up of fluid, resulting in a swelling called a cyst.
These Bartholin’s cysts are not typical and frequently develop after puberty or before menopause. About 2% of women will develop a Bartholin’s cyst in their lifetime.
Although abscesses are three times more common than cysts, Bartholin’s cysts are the most common cystic on-growths in the vulva.
A controlled case study discovered that white and black women were at a higher risk of developing Bartholin’s cyst than Hispanic women. Gradual shrinking of the Bartholin’s glands can occur when a woman reaches 30 to 35 years of age.
This may be responsible for the more frequent occurrence of Bartholin’s cyst and gland abscesses during reproductive years (between 20 and 29 years).
Causes
Medical Physiologists believe that the cause of Bartholin’s cyst is an accumulation or backed up of Bartholin’s fluid. The fluid may store up when the duct’s opening end (gland) is blocked, perhaps caused by an infection, skin flap, or injury.
Bartholin’s cyst may become infected, resulting in an abscess. An infection case of Bartholin’s cyst can be caused by several bacteria, including E.Coli and bacteria that cause sexually transmitted infections (STIs) such as Chlamydia and gonorrhea.
Risk Factors
The particular cause of the blockage of the Bartholin’s duct may not be clear. However, bacterial infections seem to play a significant role.
Individuals prone to developing a Bartholin’s cyst include those who are:
- Females.
- Sexually active.
- Between age 20 and 30 years (child-bearing age).
- Previous victims of Bartholin’s cyst.
- Patients of vaginal or vulva surgery.
- Physically traumatized or have experienced physical trauma in the affected area.
Symptoms
Bartholin’s cyst is a slow growth that ranges from pea size to as large as marble and from 0.2 to 1 inch in diameter. Small size Bartholin’s cyst may be asymptomatic (i.e., may not show any symptoms).
One cannot feel the Bartholin’s gland means a person may not realize she has a small asymptomatic Bartholin’s cyst.
In otherwise cases, when symptoms do occur, they may include:
- Redness near the opening of the vagina
- Painless, small lump near the vagina opening
- Swelling
- Discomfort during activities such as walking, sitting, or sexual intercourse.
An infected cyst is known as an abscess. If the Bartholin’s cyst becomes infected, other forms of symptoms may erupt. These include:
- Pain
- Emulsion of pus from cyst
- Fever
- Chills
- Difficulty in walking
Diagnosis
A doctor may carry out the following precise steps to diagnose a case of Bartholin’s cyst properly:
- Conduct a thorough investigation into the medical history of the patient
- Perform a pelvic exam
- Take a secretion sample from the vagina to test for any sexually transmitted infection.
- Recommend a test of the mass (biopsy test) to ascertain if the cyst is cancerous, mainly if the patient is postmenopausal or over 40 years.
If cancer is a concern, a specialist who specializes in cancer of the female reproductive system (a gynecologist) may be recommended.
Differential Diagnosis
A differential diagnosis of a disease or abnormality is a diagnosis conducted to rule out other diseases or conditions that may present similar signs and symptoms as the primary study case.
Other conditions that may resemble a Bartholin’s cyst include:
- Vaginal prolapsed
- Vulva angiomyofibroblastoma
- Endometriosis
- Choriocarcinoma
- Myeloid sarcoma
- Perineal leiomyoma
- Myxoid leiomyosarcoma
- Fibroma
- Hematoma
- Angiomyxoma
- Ischiorectal abscess
- Folliculitis
- Lipoma
- Papillary hidradenoma
- Syringoma
- Adenocarcinoma
- Squamous cell carcinoma
- Other cysts such as Gartner, Epidermal inclusion, Skene, Sebaceous, and Canal of Nuck.
Treatment
The age of a patient, infection status of the cyst, size of the cyst, and pain grade are some of the criteria that determine the approach for treating a Bartholin’s cyst.
However, if the cyst is small and asymptomatic, it may not require any treatment. If it presents symptoms, some treatment approaches include:
Medication
In cases of painful cysts, over-the-counter medications can be helpful, such as acetaminophen (Tylenol), to reduce the pain and discomfort. Doctors will prescribe antibiotics if the cyst is infected.
Surgeries
Other treatment approaches from the doctor to treat a Bartholin’s cyst. If the cyst is disturbingly large and causes symptoms, a small slit can be made by a doctor to let out or drain the accumulated fluid in the cyst. This process can be carried out in the office with the administration of a local anesthetic to the area not to feel pain.
For huge, symptomatic cysts, the doctor may insert a small tube (catheter) into the cyst and leave it in place for few weeks. A catheter allows the fluid to drain and help the duct stay open.
If the cyst continues to reoccur, a marsupialization may be conducted, and this involves making a small permanent opening that helps the fluid drain. The doctor then packs the area with special gauze to soak up the fluid and any blood; this prevents the cysts from accumulating.
This invasive process takes less than half an hour to complete. Finally, if all method fails, a doctor may recommend surgical removal of the Bartholin’s gland. However, this procedure of complete removal is rare.
Home Remedies
Home care for Bartholin’s cyst includes sitting in a warm bath two to three times daily, applying moist warm compress, which encourages fluid drainage. In several cases, home care may be enough to treat the cyst.
Complications
Most complications arise from the treatment of Bartholin’s cyst by traditional surgery. These treatments are characterized by a few disadvantages and complications such as postoperative dyspareunia, hemorrhage, infection, and the general necessity for anesthetics.
Contrary to these traditional surgeries, the CO2 laser treatment method is less invasive and more effective as it rules out these complications associated with surgery.
Prevention
There are no precise preventive measures that patients can take to avoid Bartholin’s cyst. But practicing safer sex might go a long way, like employing the idea of condoms during intercourse to avoid STIs and subsequent infection-cyst formation. Practice good hygiene.
Summary of Bartholin’s Cyst
Medical professionals have a very crucial role in the education and enlightenment of patients, especially child-bearing mothers.
Medical professionals should engage in activities, educate patients about the availability of antimicrobial agents, and provide the required information about drug-drug interaction to avoid any unknown, possibly preventable complication.
Doctors, nurses, and pharmacists must work together efficiently during women’s care with Bartholin’s cyst and other Bartholin’s gland pathologies to achieve the best treatment result for these women and their families.
Resources
- Epidemiology and differential diagnosis of Bartholin’s Cyst; https://www.nchi.nlm.nih.gov/books/NBK542271
- Treatment and complication of Bartholin’s Cyst; https://www.aafp.org/afp/2003/0701/p135.html
- Causes and Symptoms of Bartholin’s Cyst; https://www.mayoclinic.org/diseases-conditions/bartholin-cyst/symptoms-causes/syc-20369976
- Risk Factor and Diagnosis of Bartholin’s Cyst; https://www.healthline.com/health/bartholins-gland-cyst#outlook