Leptomeningeal disease (LMD) is also referred to as neoplastic meningitis, leptomeningeal metastasis, carcinomatous meningitis, meningeal metastasis, and meningeal carcinomatous.
It is a rare complication of advanced cancer disease in which malignant (cancer) cells infiltrate the layers of the central nervous system known as meninges.
Cells from some types of cancer, such as lung cancer, breast cancer, and skin cancer, may spread to the leptomeninges (comprising of pia mater and the arachnoid) which is the innermost layers of the meninges, cerebrospinal fluid (CSF), or both.
Meninges are the layers of tissue that cover and protect the brain, they are referred to as the brain jacket or spinal envelop while the cerebrospinal fluid (CSF) is a liquid found between the layers of the meninges.
This fluid is produced inside the brain and helps cushion the brain and spinal cord. A medical situation where cancer cells are found in the cerebrospinal fluid or meninges is called Leptomeningeal metastases (LM).
The leptomeningeal disease was first described by Eberth et al. in 1870 and was noted to be an uncommon complication of malignancy as it was rarely diagnosed before.
In recent times, it is estimated from 5% to 8% of patients with advanced cancer will develop Leptomeningeal disease. For patients who experience neurologic symptoms and undergo an autopsy, as many as 19% can show evidence of Leptomeningeal seeding by their cancer.
According to data from the National Cancer Institute (NCI) Surveillance Epidemiology and End Results (SEER) website, the age-fit incidence for all cancers is 461.6 per 100,000 persons per year.
Estimating 300 million as the United State population, this equates to approximately 1.4 million cancer cases and as many as 110,000 leptomeningeal cases per year.
Incidence of leptomeningeal disease occurrence is on the rise as survival for cancer patients has been extended. The longer a patient bears his or her primary cancer, the higher the prevalence of leptomeningeal disease.
The prevalence is increasing due to better imaging modalities and improved ability to treat cancer, such as with epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK) and full brain radiation.
EGFR mutations are seen in 10-15% of Caucasians and 30-40% of Asian Non-small cell lung cancer (NSCLC) cases. ALK gene rearrangements are found in 4-5% of non-small cell lung cancer cases.
Overall, 9-25% of patients with small-cell cancers demonstrate leptomeningeal disease.
Central nervous system (CNS) involvement in cancer cases is seen clinically in 30% of patients with melanoma (skin cancer) and as high as 75% at autopsy.
Although only 5% of patients with breast cancer develop leptomeningeal involvement, it remains the most common etiology of leptomeningeal disease.
The second most common occurrence of tumor with leptomeningeal disease is lung cancer. Rare tumors such as retinoblastoma and embryonal rhabdomyosarcoma can also spread to leptomeninges. Occasionally, leptomeningeal disease originating from sarcomas can also be found, though it is uncommon.
Medulloblastomaes, ependymomas, and gliomas are tumors of intracranial organ that can spread to the CSF and provoke leptomeningeal disease.
However, leptomeningeal disease remains rare in high-grade gliomas due to rapid deterioration that precludes leptomeningeal involvement.
Squamous cell carcinomas of the head and neck may likely spread to the leptomeninges (pia mater and arachnoid) along the cranial nerve tracts.
In 98% of patients with non-leukemic primary cancer, Leptomeningeal disease is accompanied by intracranial metastases.
Causes of Leptomeningeal Disease
The most common cancers to spread to the leptomeninges (pia mater and arachnoid) of the cerebrospinal fluid are breast cancer, lung cancer (both non-small and small cell), and melanoma.
Other cancers types which can sometimes develop leptomeningeal metastases include gastrointestinal, renal (kidney), thyroid, and some leukemia and lymphomas.
The leptomeninges as a component of the CNS, are more resistant to metastatic disease dueto the blood-brain barrier and the blood-CSF barrier, however, these cancer cells can bypass these barriers and reach the meninges by travelling in the blood stream (venous plexus), through hematogenous spread or direct invasion.
One possible way of entry into the CNS involves the fenestrated endothelium of the choroid plexus, which allow selective passage of solutes otherwise prohibited by intact barriers and tight junctions.
Subsequently, spread after initial leptomeningeal involvements is facilitated by constant CSF flow and regulated by various cytokines and growth factors.
Cancer cells can reach the meninges by travelling from a cancer somewhere else in the body. Or they might spread from a secondary cancer that has already developed in the brain such as in an inflammation case of the brain (encephalopathy).
A secondary cancer happens when cancer cells break away from where the cancer first started (the primary cancer) and spreads to another part of the body.
A secondary cancer is also called metastases, hence leptomeningeal metastases.
Symptoms of Leptomeningeal Disease
Leptomeningeal disease can cause many different symptoms, the most common symptoms include:
- Pain
- Seizures (a sudden attack or convulsion)
- Headaches (usually associated with nausea, vomiting, light-headedness)
- Gait difficulties from ataxia
- Memory problems
- Incontinence
- Sensory abnormalities
In some cases, less-common symptoms that may occur include:
- Double vision
- Numb chin
- Back pain
- Leg weakness
- Sphincter-related problems
- Hydrocephalus
- Loss of urine control
- Difficulty walking
Depending on the location of the tumor cells settle, leptomeningeal cancer can cause almost any neurological problems. Three affected domains of neurological function are cerebral hemisphere (15%), cranial nerves (35%) and spinal cord roots (60%).
Symptoms reported include:
- Cranial nerve abnormalities like diplopia, confusion, cognitive impairment, seizures
- Spinal symptoms like dermatomal or segmental sensory loss, neck pain, hemiparesis, limb weakness and Paresthesia
- Bowel and bladder dysfunction
- Cochlear dysfunction
- Speech difficulty
- Trigeminal sensory or motor loss
- Optic neuropathy
Diagnosis of Leptomeningeal Disease
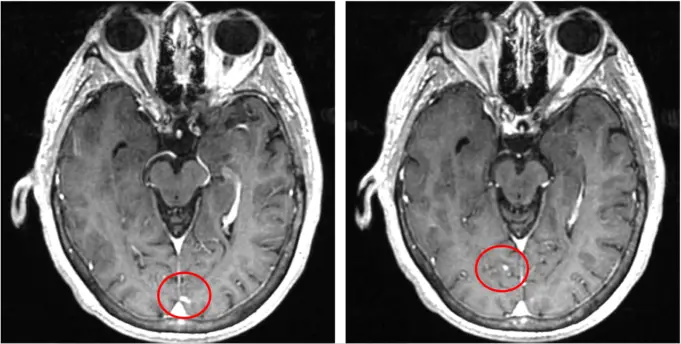
Magnetic Resonance Imaging (MRI) of the brain and spine is the ultimate standard in diagnosing leptomeningeal disease.
In some cases, the disease occurs only in the spine and not the brain, therefore a scan of the full spine and brain is very necessary. MRI can also reveal inflamed meninges and any co-existing brain metastases.
If leptomeningeal metastases are suspected, a Lumbar Puncture (Spinal Tap) is a medical procedure in which a needle is inserted into the spinal canal, in order to collect cerebrospinal fluid for diagnostic testing.
The test often recommended as the next step after an MRI. Before this test, the doctor carefully reviews the MRI to ensure that a spinal tap will be safe.
Certain findings on a spinal tap include:
- Cancer cells are not always detected, and a tap may need to be done repeatedly.
- An increased number of white blood cells (WBCs)
- An increased protein content and decreased glucose level
If intraventricular chemotherapy is considered by the clinicians, a cerebrospinal fluid flow study may be performed. This study can determine whether blockages have occurred in the flow of cerebrospinal fluid (CSF) due to the tumor.
If chemotherapy is given into an area that is blocked, it will not be effective and can be toxic.
Differential Diagnosis on Leptomeningeal Disease
Quite a number of other medical conditions can mimic leptomeningeal condition and cause similar signs and symptoms.
Some of these medical conditions include:
- Bacterial meningitis: This is a bacterial infection of the meninges; it includes meningococcal or tuberculous meningitis.
- Viral meningitis: It is also an infection of the meninges, but caused by an activity of a virus, these conditions include herpes simplex, Epstein-Barr, cytomegalovirus, varicella and zoster meningitis.
- Brain metastases: The symptoms of leptomeningeal disease and brain metastases can be very similar, and both are often diagnosed simultaneously.
- Fungal meningitis: Meninges infection by a fungus, it includes histoplasmosis, coccidiomycosis and cryptococcosis.
- Epidural or extramedullary spinal metastases
- Paraneoplastic syndromes
- Sarcoidosis
- Toxic (metabolic) encephalopathy: Drug induced encephalopathy, often due to anti-cancer drugs, antibiotics or pain medications, can create similar symptoms of leptomeningeal metastases.
Leptomeningeal Disease Treatment
Leptomeningeal disease treatment depends on severity of symptoms, primary cancer involved, and general well-being of the patient and presence of other metastases.
Leptomeningeal metastases are very challenging to treat due to the often occurrence in advanced stages of cancer and after a person has been sick for a significant period of time, creating a situation of unknown life expectancy of the patient and resulting in unconfirmed prognostic data of the condition.
Due to this reason, the major goal of treatment for leptomeningeal disease is to relieve symptoms and attempt to destroy cancerous cell growth in the meninges and cerebrospinal fluid (CSF).
Radiotherapy, chemotherapy or both may be recommended by the doctor depending on the situation of the condition. Treatment plan are usually discussed with patients and their families for adequate preparations.
A patient may get Radiation therapy to places where clusters of cancer cells are causing symptoms, such as the head, areas on the spinal cord or to both. In some radiotherapy treatment, one area is treated first and the other area later.
Chemotherapy treatment for leptomeningeal disease exists in three different ways:
- Oral chemotherapy (pill swallowing)
- Intravenous (IV) chemotherapy (through a needle to the vein)
- Intrathecal chemotherapy or intra-ommaya chemotherapy (Directing into the CSF)
The doctor chooses the best form of chemotherapy administration. Different types of cancer respond best to different types of chemotherapies.
If a patient is getting chemotherapy directly into the cerebrospinal fluid (CSF), it will probably be done with an Ommaya reservoir. An ommaya reservoir is a dome shaped device that is placed under the scalp during a surgery.
It has a small tube that connects it to the areas of the brain where CSF is produced. Chemotherapy given this way has a very few side effects because only a small dose is needed to treat the cancer cells in the CSF.
But even when patients have an Ommaya reservoir, they might also get intrathecal chemotherapy through a lumbar puncture, IV chemotherapy or oral therapy. This is to help control both the primary cancer and the leptomeningeal metastases.
However, there are some risks during the course of the treatments; both chemotherapy and radiotherapy are harmful to the body and most definitely the brain and spinal cord. Caution must be utilized in treating patients with leptomeningeal disease.
Another factor that makes treatment of leptomeningeal metastases difficult is that there is no favorable method to evaluate the disease progression.
Management
There are numerous ways that symptoms of leptomeningeal metastases can be managed. It is important to inform a clinician about any issues, changes or improvement in symptoms.
This will assist and update the doctors and nurses about the patient’s condition and the effectiveness of treatment. Being diagnosed with a complication such as leptomeningeal metastases might cause anxiety in patients, so doctors are always on alert if a patient wants to discuss concerns about leptomeningeal disease, primary cancer, or both. In some other cases, palliative care can still help greatly with managing symptoms.
Many cancer centers now have palliative care teams that work with cancer patients to ensure they have the best possible quality of life while living with the disease.
People do not have to possess terminal cancer to receive a palliative care consult: This aspect of care can be beneficial even with early-stage and highly curable cancers.
Summary
Leptomeningeal disease also known as neoplastic meningitis or carcinomatous meningitis, is a rare medical complication of advanced cancer conditions.
It occurs when cancer cells affect the cerebrospinal fluid or meninges; the layer covering the spinal cord and brain. The leptomeningeal disease may occur when cancerous cells spread or migrate from a primary site of cancer infection either in the brain or from other parts of the body such as from areas of lung cancer, breast cancer, skin cancer, and so on.
Leptomeningeal disease can cause a variety of neurological symptoms from vision impairment to locomotive difficulties, depending on the loci point of the tumor.
It usually diagnosed using MRI and cerebrospinal fluid flow study. The condition does not have a universal cure and so like other forms of cancer, its progression and symptoms are usually treated, though some treatment approach like radiotherapy and chemotherapy have medically proven to slow the progression of leptomeningeal disease.
The disease is referred to as a deadly condition because of its onset only in cases of advance cancer, not giving enough time or for study and not favoring treatments on long-term basis. But with prompt attention to the condition and cooperation of patients, leptomeningeal disease can adequately be managed.
Sources;
- Radiotherapy in Leptomeningeal Disease; https://www.frontiersin.org/articles/10.3389/fonc.2019.01224/full
- Leptomeningeal Disease; http://www.mountsinai.org/care/neurosurgery/services/brain-tumors/leptomeningeal-disease
- leptomeningeal disease care; http://www.mdanderson.org/cancerwise/new-hope-for-leptomeningeal-disease-care.h00-159144456.html
- Leptomeningeal Disease; http://www.hindawi.com/journals/crionm/2020/6349456/