Angina is chest pain that occurs as a result of reduced blood flow to the heart. Symptoms of angina feel similar to those of a heart attack, with pressure and squeezing in the chest. Angina is sometimes known as ischemic chest pain or angina pectoris.
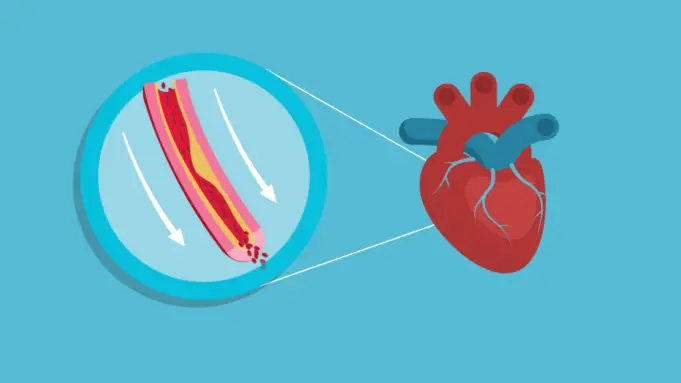
Angina is a symptom of a heart disorder and occurs due to blockage of the arteries or as a result of insufficient blood flow to the arteries that transport oxygen-rich blood to the heart.
Angina typically goes away quickly. However, it can still be a sign of a life-threatening heart disorder. Finding out the cause of this symptom is vital in order to avoid a heart attack.
Medication and changes in lifestyle can control the impact of angina. In more severe cases, surgery may be required. There might also be a need to insert a stent – a tiny tube that props open arteries – into the heart.
Types of Angina
- Stable Angina: This is the most common type of angina. It can be triggered by stress or physical activity. Stable angina typically lasts for a few minutes and goes away after the body rests. It is not a heart attack, but it can be a sign of a likely heart attack. It is necessary to seek medical attention if you experience one.
- Unstable Angina: Unstable angina can occur while the body is inactive or at rest. The pain can be severe and long-lasting and may happen several times. It is often a sign of a heart attack and needs to be checked by a doctor as soon as possible.
- Microvascular Angina: This type of angina occurs with chest pain but no blockage in the arteries. It happens as a result of impaired coronary arteries. These small arteries do not work as well as they should, causing an inadequate supply of blood to the heart. The chest pain usually lasts for more than 10 minutes. A person may also experience associated symptoms such as shortness of breath, irregular sleep patterns, fatigue, and low energy. Microvascular angina is more common in women.
- Prinzmetal’s Angina: This is also known as variant angina and is very rare. It may occur while the person is asleep at night or while at rest. Prinzmetal angina causes the arteries to narrow or tighten suddenly. This can cause a lot of pain and should get treated immediately.
Causes and Risk Factors of Angina
Causes of angina include:
- Coronary microvascular disease: Occurs when the small arteries of the heart become damaged, resulting in reduced blood flow.
- Coronary artery disease: This occurs when a substance called plaque builds on the walls of the arteries of the heart, causing them to narrow.
- Blood clots: Blood clots form in the arteries around the heart in cases of unstable angina. These clots partially or entirely block the flow of blood in an artery, which leads to angina symptoms and possibly a heart attack.
Risk factors that can trigger symptoms of angina include:
- Diabetes: This condition increases the risk of coronary artery disease, which leads to angina and heart attacks by increasing cholesterol levels.
- High blood cholesterol or triglyceride levels: Cholesterol forms a significant part of the deposits that can narrow arteries in the body, including those that supply the heart. A high amount of low-density lipoprotein (LDL) cholesterol, also known as “bad” cholesterol, increases one’s risk of angina and heart attacks. An increased level of triglycerides, a type of blood fat related to diet, is also unhealthy.
- Tobacco: Chewing, smoking, and long-term exposure to secondhand smoke from tobacco can damage the inside of the arteries — including arteries to your heart. This allows deposits of cholesterol to collect and block the flow of blood.
- High blood pressure: An increased blood pressure damages arteries over time by accelerating the hardening of the arteries.
- Obesity: Obesity is often associated with high blood cholesterol levels, high blood pressure, and diabetes, all of which increase the risk of angina and heart disease. An overweight person’s heart has to work harder to supply blood to the body.
- Family history of heart disease: You’re at a greater risk of developing angina if a member of your family has coronary artery disease or has had a heart attack.
- Age: Men older than 45 and women older than 55 have a greater risk than younger adults.
- Stress: Stress can increase the risk of angina. Stress, as well as anger, also can raise blood pressure. Surges of hormones produced during stress can narrow the arteries and worsen angina.
- Lack of exercise: A sedentary lifestyle contributes to high cholesterol, high blood pressure, type 2 diabetes, and obesity. However, it is important to talk with your doctor before starting an exercise program.
Sign and Symptoms of Angina
Symptoms of angina include any of the following sensations in the chest:
- Pressure
- Tightening
- Squeezing
- Burning or aching across the chest, usually originating behind the breastbone
- Heaviness
Pain from the chest often spreads to the neck, shoulders, arms, jaw, throat, teeth, or back.
Other possible signs of angina include:
- Fatigue and weakness
- Heartburn
- Nausea
- Cramping
- Indigestion
- Shortness of breath
- Sweating
The duration of these signs depends on the type of angina.
Seek immediate medical attention if you develop any of these symptoms.
Symptoms in Women
Symptoms of angina may differ between men and women. Some women may not feel the classic symptoms of chest tightness and pressure but can sometimes feel only fatigue due to the condition.
Women are also more likely to develop coronary microvascular disease (CMD), a condition that involves the blockage of the tiny arteries in the heart, limiting blood flow.
CMD is different from coronary artery disease, which occurs due to the buildup of plaque that restricts blood flow. 50% of women with symptoms of angina don’t have a major coronary artery blocked, according to the American Heart Association.
Women that have CMD often experience microvascular angina, which can occur during routine activities as well as with physical or mental stress.
Diagnosis
Your doctor will begin the diagnosis by conducting a physical exam and making inquiries about your medical and family history.
Other tests your doctor may order to help confirm the presence of angina include:
- Electrocardiogram (ECG or EKG): This machine records electrical signals as they travel through the heart. This would help the doctor find patterns in these heartbeats to see if the blood flow through the heart has been slowed or interrupted or if you’re having a heart attack.
- Cardiac MRI: In a cardiac MRI, detailed images of your heart’s structure and blood are produced when you lie on a table inside a long, tubelike machine.
- Echocardiogram: This machine uses sound waves to produce images of the heart. The doctor can use these images to identify angina-related issues, including heart muscle damage due to low blood flow. An echocardiogram can be carried out alongside a stress test, and this can show if there are areas of the heart that are not getting enough blood.
- Cardiac computerized tomography (CT) scan: In this procedure, images of the heart and chest are collected. These images show if any of the heart’s arteries are narrowed or if the heart is enlarged.
- Stress test: Angina is sometimes easier to diagnose when the heart is working harder. A stress test would require the patient to walk on a treadmill or pedal a stationary bicycle. Blood pressure and ECG readings are observed as the exercise continues. Other tests also may be done alongside a stress test.
- Blood tests: Certain heart enzymes slowly leak into the blood if the heart has been damaged by a heart attack. Blood samples can be tested for the presence of these enzymes.
- Chest X-ray: This test takes images of the heart and lungs. This is to discover other conditions that might explain symptoms and see if you have an enlarged heart.
- Coronary angiography: This procedure involves using X-ray imaging to examine the inside of the heart’s blood vessels. It’s part of a general group of practices known as cardiac catheterization. During coronary angiography, a type of dye visible by an X-ray machine is injected into the heart’s blood vessels. The X-ray machine rapidly takes a series of images, also known as angiograms, offering a detailed look at the insides of the blood vessels.
Treatment
The aim of treatment is to reduce pain, prevent symptoms and prevent or lower the risk of heart attack, This would involve lifestyle changes, medication, surgery, or a combination of all of them.
Lifestyle changes
The following can help:
- Resting where necessary
- Stopping smoking
- Getting regular exercise
- Avoiding stress and its triggers
- Regular checking of cholesterol levels
- Eating a healthy diet
- Maintaining a healthy weight
Medications
Nitrates are often prescribed by doctors to treat angina symptoms. They work by reducing the intensity of angina by relaxing and widening the blood vessels.
Other drug options include:
- Beta-blockers
- Oral antiplatelet medications
- Angiotensin-converting enzyme inhibitors
- Calcium channel blockers
- Statins, which are cholesterol-lowering medicines
- Anticoagulants
Sources
- Angina (Symptoms, Causes, Types, Diagnosis, and Treatment) – MedicineNet
- Angina – MayoClinic
- Everything you need to know about angina – MedicalNewsToday
- All About Angina – Healthline
- Angina in Women Can Be Different Than Men – Heart.org