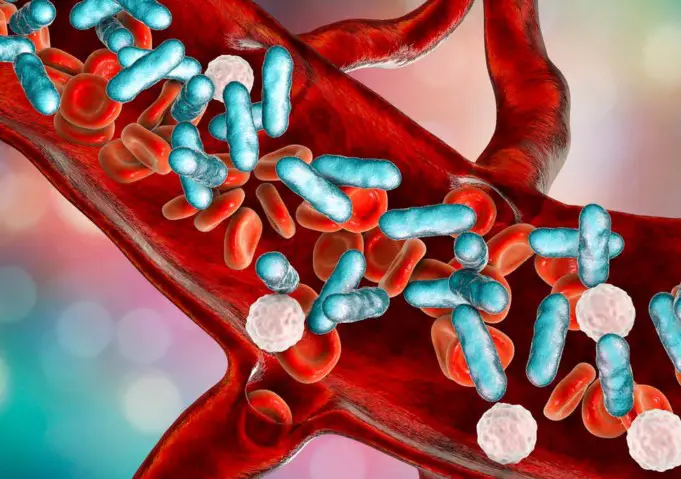
Sepsis is a severe and life-threatening condition caused by the body’s response to infection, which leads to severe damage to tissues and organ failure.
Although sepsis is commonly interchanged with septicemia, it differs from the latter in that septicemia is the poisoning of the blood by bacteria. Hence, septicemia leads to sepsis.
Sepsis occurs when the immune system mounts a tremendous inflammatory defense in response to these poisons. A large amount of chemicals released into the bloodstream by the immune system triggers inflammation, which leads to damage to organs.
The flow of blood to the limbs and internal organs is reduced due to blood clotting, and this leads to a corresponding reduced flow of nutrients and oxygen which causes organ failure in severe cases.
The common symptoms of this condition include increased heart rate, fever, increased breathing rate, and confusion. Other symptoms include painful urination caused by kidney infection and pneumonia.
People with a weakened immune system, the aged and young children, may show no visible signs and may have normal body temperature. Severe sepsis may lead to low blood pressure, high blood lactate levels, and septic shock.
Although viral, fungal, and protozoan infections may lead to sepsis, bacterial infections are the most common cause of sepsis. The most common areas of the body that could be primarily infected are the brain, lungs, abdominal organs, and urinary tract.
The risk of death from severe sepsis is as high as 50%, while that of septic shock is as high as 80%. It has been estimated that sepsis affects millions of people annually, although the exact number of cases worldwide is unknown. Sepsis is known to occur more in males than in females.
Causes and Risk Factors of Sepsis
Although bacterial infections are the most common causes of sepsis, the condition can occur as a result of other diseases. It can start anywhere where viruses and bacteria enter the body.
Sometimes it could be caused by something as minor as a bruised knee or a cut on the hand. Medical conditions that could put one at risk include:
- Gas gangrene, cellulitis, necrotizing fasciitis and myonecrosis that affect the skin
- Sinusitis, pharyngitis, tonsillitis and other upper respiratory tract infections
- Pneumonia, chest pain and lung abscess in the lower respiratory tract
- Inflammation, erythema, edema and discharge of pus from infected wounds
- Meningitis, infected hematoma, brain abscess in the central nervous system
- Ruptured brain aneurysm
- Colitis, diarrhea, appendicitis, abdominal pain with vomiting occurring as a result of bacterial infection such as Escherichia coli, Salmonella, Shigella, Campylobacter, or Clostridium difficile
- Pancreatitis, liver abscess, perforation of the abdomen, pyelonephritis, and cholecystitis
- Osteomyelitis with pain, swelling, warmth and decreased movement
- Septic arthritis with pain, swelling, heat and reduced movement
- Other diseases such as Lyme disease, Babesiosis, typhoid fever, and rickettsial diseases
Specific populations are at risk of developing sepsis. They include:
- People with compromised immune systems such as those living with HIV/AIDS or Cancer
- The old, especially those with other health problems
- Infants
- Diabetic patients
- People who have recently undergone major surgery
- People that consume immune system suppressing drugs like steroids
Signs and Symptoms of Sepsis
Two of the following symptoms must be observed before sepsis can be confirmed:
- Fever with a temperature above 38ºC or below 36ºC
- Breathing rate more than 20 breaths per minute
- Heartbeat rate higher than 90 beats per minute
- Probable or confirmed infection
Severe sepsis occurs when there is organ failure. For severe cases of the condition to be diagnosed, two of the following symptoms must be confirmed:
- Extreme exhaustion and fatigue
- Decreased urination
- Reduced mental ability
- Decreased platelet count
- Chills and shivering due to reduced body temperature
- Patches of discolored skin
- Difficulty breathing
- Abnormal heart functions
- Unconsciousness
- Altered functioning of liver or kidneys
- Low blood pressure
- High or low white blood cells
- Slurred speech
- Diarrhea, nausea, and vomiting
What is Septic Shock?
Septic shock is a potentially fatal condition that occurs when sepsis leads to dangerously low blood pressure. When the symptoms of a septic patient with low blood pressure do not improve with fluid treatment, it means that their body has gone into septic shock.
They would require medications known as vasopressors to keep their blood pressure high and improve blood flow through the organs.
Lack of this particular treatment may cause insufficient blood flow in the body that can cause the failure of organs such as the lungs, kidneys, heart, and brain.
Septic shock is a serious condition that can cause chronic pain, incorrectly functioning organs and post-traumatic stress disorder (PTSD)
Diagnosis of Sepsis
If you present symptoms of sepsis, your doctor may require tests to confirm the diagnosis and determine the severity of the infection.
Blood tests would be needed to check for complications like infections, decreased amount of oxygen, problems with blood clotting, abnormal kidney and liver function, and electrolyte imbalance, which affects the amount of water and acid level in the blood.
Other tests include;
- Urine test (to check for possible bacteria in your urine)
- Mucus secretion test (to identify microorganisms responsible for an infection)
- Wound secretion test
In the event that the source of infection cannot be determined with the tests above, an internal image of your body may be necessary for diagnoses.
X-rays would be used to view the lungs, ultrasounds to view infections in the gallbladder and ovaries, MRI to scan soft tissues for possible infections, and CT scans to see infections in the pancreas, appendix and bowel area.
Treatment
Sepsis is a life-threatening illness that requires immediate and intensive medical attention. People with sepsis and septic shock need to be hospitalized for close monitoring and treatment.
The following medications are used to treat sepsis:
Antibiotics
Treatment of diagnosed septic patients should begin within the first 6 hours after diagnosis. Antibiotics would be administered intravenously (directly into the vein).
Broad-spectrum antibiotics that act against bacteria would be used until blood tests reveal which bacteria, in particular, is responsible for the infection.
Vasopressors
These medications are needed to maintain adequate blood pressure in people with septic shock. This would be necessary if, after fluid treatment, blood pressure remains low.
Vasopressors increase blood pressure by tightening the blood vessels. If the blood pressure continues to drop with this medication, the situation is a cause for concern.
Corticosteroids
Doctors use these when blood pressure and heart rate continue to be unstable even after they have received fluid treatment and vasopressors.
People with severe sepsis and septic shock would require attention in an intensive care unit (ICU) as they may need oxygen, intravenous (IV) fluids, mechanical ventilation, and vasopressors.
Prevention
- Get regular vaccinations against diseases such as chickenpox, flu, pneumonia, and other viral infections that may lead to sepsis
- Avoid smoking
- Practicing good hygiene is vital for the prevention of sepsis. Bathing and changing clothes regularly, frequent washing of hands, especially before and after handling of food, using the bathroom, and touching pets are necessary to prevent infection.
- Care for and clean any open wounds. Clean wounds with soap-free water and see a doctor if the wound does not seem in a few days.
- Be on the lookout for signs of infection, such as chills, fever, rapid breathing, rash, or confusion.
- Finish any antibiotic medication given to you by your doctor after a bacterial infection to keep future infections at bay.
- Treat parasitic and fungal infections as soon as symptoms appear, and use medication specific to the particular fungus or parasite.