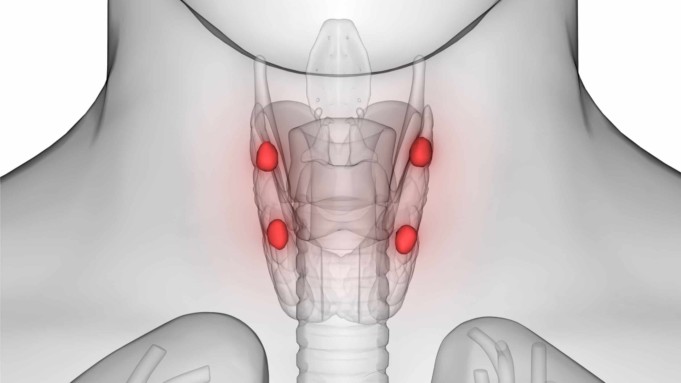
In humans there are four pea-sized parathyroid glands embedded in the thyroid gland, these organs all form a butterfly-shaped that consists of two lobes located at either side of the trachea (windpipe).
They are all located in the neck region of the human body just at the front below the larynx (Adam’s apple). Even though their names seem very similar, the parathyroid and thyroid gland have different functions.
The parathyroid glands produce only one hormone called parathormone (PTH) which is a peptide composed of 84 amino acids. Parathormone and thyroid hormone calcitonin, work antagonistically (in opposite ways) to regulate the calcium and phosphate levels of the blood. The release of parathormone increases the calcium level to its normal level and decreases the phosphate level.
The activity of the parathyroid glands is controlled by a simple negative feedback mechanism. Hyperactivity of the gland reduces the level of calcium in the blood and tissues due to calcium excretion in urine.
This can lead to a state of tetany in which muscles remain contracted, also the rate of excretion of phosphate is reduced and the level of phosphate ions in the blood rises.
Parathyroid Disease
Parathyroid disease is basically an abnormality in the function or structure of the parathyroid gland. There are three types of parathyroid diseases, which are hypoparathyroidism, hyperparathyroidism, and parathyroid cancer. The most frequent type of parathyroid disease with the highest statistical number is hyperparathyroidism.
Hyperparathyroidism is the condition that occurs when a parathyroid gland begins to excessively secrete parathyroid hormone, resulting in a rise in the levels of calcium in the bloodstream.
On the other hand, if the parathyroid hormonal secretion is lower than the normal/required levels, it will lead to low levels of calcium in the blood, this situation is called hypoparathyroidism.
In some cases, it is also possible that a benign tumor growth situated on a parathyroid gland makes it overactive and bigger in size. In very rare cases, hyperparathyroidism can be caused by parathyroid cancer.
Parathyroid diseases affect the brain, bones, kidneys, gastrointestinal tract, nervous system, muscles, blood vessels, and heart, the risk of certain cancer might even be increased.
Signs and Symptoms of Parathyroid Disease
Depending solely on the parathyroid disease presented, symptoms may vary greatly, that is, they vary depending on the type of parathyroid disease.
The most common symptoms of hyperparathyroidism include:
- Chronic fatigue
- Difficult or lack of sleep
- Irritability/Crankiness
- Headache
- Body aches
- Bone pain
- Poor concentration
- Memory loss
- Depression or anxiety
If the condition is left unattended to, it can also lead to more severe symptoms such as:
- Cardiac arrhythmias
- Osteoporosis and Osteopenia
- Hypertension
- Kidney stones
- Kidney failure
- Gastric acid reflux resulting in heartburns.
- Low libido (sex drive)
- Thinning hair (predominately in middle-aged females on the front part of the scalp)
- High liver function test
- Development of MGUS and abnormal blood protein levels
Signs and Symptoms of hypoparathyroidism may include:
- Fatigue or general weakness of the body
- Patchy hair loss
- Tingling or burning sensations in fingertips and toes and lips
- Muscular aches and cramps in legs, feet, stomach, or face
- Muscle spasms
- Brittle nails
- Anxiety or depression
- Painful menstrual periods for women
- Patchy high losses are sometimes seen.
Signs and Symptoms of parathyroid cancer include weakness, feeling tired, and feeling of a lump in the neck, others may include:
- Vomiting
- Constipation
- Constant urination
- Weight loss
- Loss of appetite
- Confusion
- Bone pain
- Hoarseness (causes by cancer invading the vocal cords or their nerves)
- Swallowing difficulty
- Pain in the back or side and blood in the urine due to the development of kidney stones
Causes of Parathyroid Disease
Hyperparathyroidism is caused by series of factors that increase the production of parathyroid hormone. Hyperparathyroidism is classified into three different classes, base on the cause of the condition:
Primary hyperparathyroidism
Primary hyperparathyroidism occurs due to some problems with one or more of the four parathyroid glands. Conditions that can cause this include:
- Enlargement of two or more parathyroid glands (hyperplasia), accounts for most other cases about 15% of cases.
- About 80% of cases of hyperparathyroidism is caused by an adenoma (noncancerous growth) on a gland
- Primary hyperparathyroidism usually occurs randomly, but some people inherit genes that can lead to the disorder.
- Secondary hyperparathyroidism
Secondary hyperparathyroidism is the result of other conditions that lower the calcium levels in the blood. This causes an overworking of the parathyroid gland in order to compensate for the calcium loss. These factors include:
- Severe vitamin D deficiency: Vitamin D helps maintain appropriate calcium levels in the blood. It also assists the digestive system to absorb calcium from food. Sunlight and diet are the major sources of vitamin D but if the body does not get enough vitamin D, calcium levels will drop.
- Severe calcium deficiency: The body may lack calcium or may not get enough calcium from the diet, often due to the inability of the digestive system to absorb calcium from the diet.
- Chronic kidney failure: Conversion of absorbed vitamin D to forms that can be utilized by the body system is one of the primary functions of the kidney. But if the kidney is poorly functioning or infected, usable vitamin D may decline and calcium levels will drop. Chronic kidney failure is the most common cause of secondary hyperparathyroidism.
- Tertiary hyperparathyroidism
These are very rare. In some patients with long-term end-stage kidney disease, the parathyroid glands enlarge and begin to release parathyroid hormones on their own and parathyroid hormone does not go down with medical treatment.
Hypoparathyroidism, on the other hand, occurs when the parathyroid gland does not secrete enough parathyroid hormone. Factors that can cause this condition include:
- Neck surgery: The most common cause of hypoparathyroidism develops after accidental damage to or the total removal of the parathyroid gland during surgery. These neck surgeries may include treatment of the thyroid gland or treatment of throat or neck cancer.
- Hereditary hypoparathyroidism: This includes those born with incomplete parathyroid glands or improper functioning parathyroid glands. Some types of hereditary hypoparathyroidism are associated with deficiencies of other hormone-producing glands.
- Autoimmune disease: These are situations where the immune system identifies the parathyroid tissues as foreign bodies and attacks parathyroid tissues. In this situation, the parathyroid glands stop secreting their hormone.
- Low levels of magnesium: Magnesium is required at a normal level for the normal production of parathyroid hormone. If these magnesium levels are low, it can drastically affect the function of the parathyroid glands.
- Extensive cancer radiation treatment of the neck: Adverse Radiation treatment can result in the destruction of the parathyroid glands.
Some possible causes of parathyroid cancer include:
- Radiation: treatment with X-rays or other kinds of energy to the neck.
- MEN1 syndrome (Multiple Endocrine Neoplasia type 1): a condition connected to tumors of hormone-producing glands.
- Familial Isolated Hyperparathyroidism: a condition that can cause kidney stones, nausea, high blood pressure, vomiting, and fatigue.
Risk factors
Increased risk of primary hyperparathyroidism may occur if a person:
- Have had prolonged severe calcium or vitamin D deficiency.
- Is a woman who has gone through menopause?
- Have had radiation treatment for cancer that has exposed the neck to radiation.
- Have inherited rare disorders such as Multiple Endocrine Neoplasia type 1, which always affects multiple glands.
- Is on lithium medication; a medication used most often to treat bipolar disorder.
Factors that can increase the risk of developing hypoparathyroidism and parathyroid cancer include:
- A family history of the condition
- Having certain autoimmune or endocrine conditions such as Addison’s disease, which causes a decrease in the hormone the adrenal glands secrete.
Diagnosis of Parathyroid Disease
Most people with parathyroid disease visit the doctor because they feel they have kidney issues or bone problems or even both. Parathyroid disease is usually diagnosed by testing the levels of calcium and parathyroid hormone in the blood.
Once the diagnosis is completed, the doctor may counsel for more tests to check and cross-check any other possible causes. This helps the severity of the condition, tests usually include bone densitometry, Parathyroid scan, CAT scan, MRI scan, Angiogram, an ultrasound scan of the kidneys, and a 25-hydroxy-vitamin D blood test.
Complications of Parathyroid Disease
Complications of Hyperparathyroidism are mainly related to the long-term effects of too little calcium in the bones and too much calcium in the bloodstream.
Common complications include:
- Osteoporosis: Weak, brittle bones that fractures easily due to loss of calcium in the bones
- Kidney stone: Too much calcium in the bloodstream may lead to too much calcium in the urine, which can result to small, hard deposits of calcium and other substances to form in the kidneys.
- Neonatal hypoparathyroidism: Severe, untreated hyperparathyroidism in pregnant women may cause dangerously subsequent low levels of calcium in newborns.
- Cardiovascular disease complications
Hypoparathyroidism can result in various complications both reversible and irreversible such as:
Reversible complications
Cramp-like spasms that can be prolonged and painful, occurs in the face, throat, and arms. When it occurs in the throat, it can interfere with breathing, creating a possible emergency.
- Tingling or burning sensations in the lips, tongue, finger, and toes
- Seizures
- Malformed teeth; affecting dental enamel and root at an early stage of teeth development.
- Kidney problems
- Heart arrhythmias and fainting
Irreversible complications
- Stunted growth
- Slow mental development in children
- Vision impairment due to cataracts
- Calcium deposits in the brain can cause balancing problems and seizures.
The most serious complication of parathyroid cancer is hypercalcemia. Most death from parathyroid cancer occurs as a result of severe difficult-to-control hypercalcemia and not cancer itself.
Other complications may include:
- Poor appetite
- Constipation
- Abnormal fractures
- Frequent thirst
- Bone pain
- Nausea and vomiting
Treatment of Parathyroid Disease
Treatment options for parathyroid diseases include monitoring, medication, dietary supplements and surgery. Surgery has been discovered to be the most effective option to treat the disease. It entails removal of overactive parathyroid glands and can be performed either in a minimally invasive way or by a standard neck exploration.
Even though potential complications from this surgery are rare, some patients may experience damage to the nerves controlling their vocal cords after the surgery and it may affect speech. Also, once the surgery is successfully completed, the patients may need to take calcium and vitamin D medications so that their blood calcium levels remain normal.
On the other hand, if a patient experiences a mild primary parathyroid disease, he/she may only need proper monitoring. Monitoring usually consists of carrying out bone density measurements, physical exams, blood tests for calcium levels, and kidney function tests from time to time.
Sources;
- Parathyroid Cancer; http://www.webmd.com/cancer/parathyroid-cancer
- Parathyroid Disorders; https://medlineplus.gov/parathyroiddisorders.html
- Parathyroid Disorders; https://www.uofmhealth.org/conditions-treatments/endocrinology-diabetes-and-metabolism/parathyroid-disorders
- Hyperthyroidism;https://www.mayoclinic.org/diseases-conditions/hyperparathyroidism/symptoms-causes/syc-20356194