Gastrectomy is a major surgical procedure where all or part of the stomach is removed and is mostly recommended for life-threatening conditions such as stomach cancer.
Partial or total removal of the stomach doesn’t take away one’s ability to digest liquids and foods, although several lifestyle changes may be needed after the procedure.
When is gastrectomy is needed?
Your doctor may recommend gastronomy if you’re suffering from a stomach condition that isn’t responding to other known treatments. It is mostly used to treat:
- Noncancerous, or benign tumors
- Bleeding
- Inflammation
- Polyps, or growths inside your stomach
- Perforations in the stomach wall
- Stomach cancer
- Duodenal or severe peptic ulcers
It can also be instrumental in treating obesity. Making the stomach smaller means it fills more quickly, and this helps an individual eat less. However, gastrectomy is only used to treat obesity when other options have failed.
Less invasive obesity treatments include;
- Diet
- Exercise
- Medication
- Counseling
Types of gastronomy
There are three primary types of gastrectomy operations, depending on which part of your stomach needs to be removed:
Partial gastrectomy
This is the removal of a part of the stomach. The lower half of the stomach is usually removed. An incision is made in the abdomen, and surgical instruments are passed through it to access and remove the lower part of the stomach.
After which the remaining upper portion of the stomach is connected to the small intestine
Total gastrectomy
This involves the removal of the whole stomach. An incision is also made in the abdomen, and the stomach is removed through it. The esophagus is then attached to the small intestine.
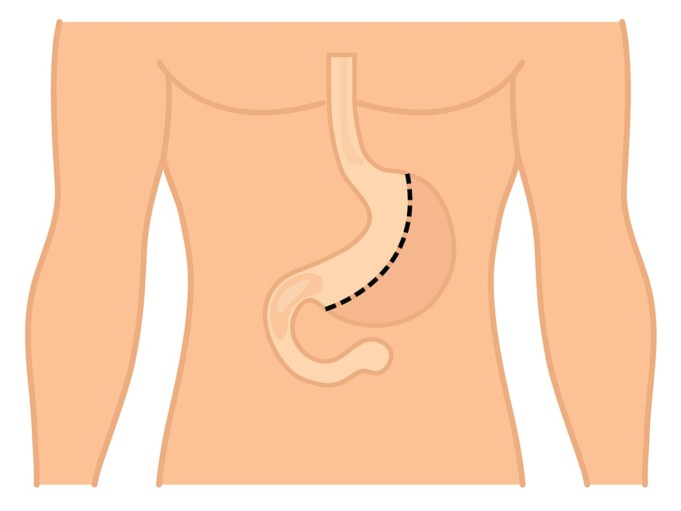
Sleeve gastrectomy
This is the removal of the left side of the stomach and is usually performed as part of a surgical procedure for weight loss. Around 80% of the stomach is removed in this process, usually through keyhole surgery.
A tube or sleeve is then placed in the position where the stomach occupies, and it acts as the new stomach, it is positioned upwards and sealed with stitches. The tube or sleeve usually has a capacity of 100mL – 200mL; this significantly reduces the amount of food one needs to eat in order to feel full.
How is gastrectomy performed?
Gastrectomy Operations of all kinds are performed under general anesthesia, so an individual could be induced with a medication that makes them fall into a deep sleep during the operation and so they won’t be able to feel any pain.
Gastrectomy is performed using one of the following techniques:
Open surgery
This method involves cutting the skin and tissues to create an opening so the surgeon can have a full view of the structures and organs involved. This surgery involves a single, large incision. The surgeon pulls back skin, muscle, and tissue to access the stomach.
Laparoscopic surgery
Laparoscopic surgery is minimally invasive, as it involves small incisions and specialized tools. The procedure is less painful, it heals faster, and patients recover on time. It’s also called “keyhole surgery” or laparoscopically assisted gastrectomy (LAG).
Laparoscopic surgery is usually preferred to open surgery because it is a more advanced surgery, and complication rates are lower. But for certain conditions like stomach cancer, doctors may recommend open surgery over laparoscopic surgery.
It is wise to discuss the advantages and disadvantages of both with your surgeon before deciding which procedure to have
How to prepare for gastrectomy
Blood tests and imaging tests are usually requested by your doctor or surgeon before the surgery. A complete assessment of your medical history is also required, so it is vital that you tell your doctor about any medical issues or ailments you may have had or are currently experiencing or if you’re taking any medications.
People who smoke cigarettes are usually told to stop smoking as it can cause more complications and may prolong recovery.
Recovering after a gastrectomy operation
Since gastrectomy is a major operation, recovery may take a long time, and so you’ll have to remain at the hospital for about 1 or 2 weeks after the procedure.
You may be given nutrition directly into a vein until you can eat and drink again, and you will be able to digest most foods and liquids, but you may have to make some changes to your diet.
Potential risks of a gastrectomy include the following:
- Acid reflux
- Diarrhea
- Gastric dumping syndrome (a severe form of maldigestion)
- Internal bleeding
- Leaking from the stomach at the operation site
- Nausea
- An infection of the incision wound
- An infection in the chest
- Vitamin deficiency
- Vomiting
- Stomach acid leaking into your esophagus (which causes scarring, narrowing, or constriction)
- A blockage of the small bowel
- Loss of weight
- Constant bleeding
- Difficulty in breathing
- Pneumonia
- Damage to adjacent structures
Before signing up for the operation, your doctor should be aware of your medical history and what medications you’re currently on. Follow all instructions you’re given while preparing for the procedure to minimize your risks.
Life after gastronomy
Once the incisions are closed with stitches and wounds bandaged, you’ll be required to remain in the hospital for one or two weeks to heal and recover.
You will likely have a tube running from your nose to your stomach during this period, which allows the doctors and nurses to remove any fluids produced by your stomach, and it keeps you from feeling nauseated.
You will be fed through a tube attached to one of your veins until you’re healed enough to eat and drink normally. Do not hesitate to seek immediate medical attention if you develop any new symptoms or pain.
What lifestyle changes are required?
Once you’re strong enough to return home, you may have to change or adjust your eating habits. These changes may include:
- Eating smaller food rations throughout the day
- Avoiding foods with high fiber
- Taking vitamin supplements
- Eating foods rich in iron, calcium, and vitamins C and D
It takes a long time to recover from gastronomy. Eventually, your small intestine and stomach will stretch. Then, you’ll be able to eat more substantial meal portions and more fiber.
You’ll need to undergo regular blood tests after the surgery to make sure that you’re getting adequate vitamins and minerals.
References;
- Gastronomy – NHS
- Sleeve gastronomy – MayoClinic
- Stomach Polyps – MayoClinic