White matter disease is also referred to as multiple cerebral infarctions, white matter dementia or leukoaraiosis. White matter disease is a disease condition of the nervous system that is categorized by the wearing out or degeneration of the white matter of the brain.
Simply put the brain and spinal cord are both made up of cells known as neurons or nerve cells. White matter is the area of the brain that is made up of mainly myelinated axons, which are long relays that extends out from the soma and it is white in color due to the high lipid fat content of the myelin protein that sheathes them.
The white matter is a portion where brain cells meet with nerve cells (neurons) from the spinal cord.
The white matter contains fatty tissues called myelin, these myelin covers and protects the axons (the extended arms of neurons), the axons of the brain cells connect to the axons of the spinal cord and these connections facilitates the bio-electrical transmission of nerve signals, thereby enabling quick communication (stimulation and response).
Destruction or degeneration of the white matter can be a result of so many factors; from infection to genetic factors, however, this degeneration (especially white matter surrounding the myelin sheaths) can affect a person’s locomotive response, visual and auditory system and can lead to neurological complications.
Behavioral neurology is simply known for a long time as the study of the higher cortical function. The relationship between abnormal cognitive behavior and degeneration of some part of the cortex of the brain has been supported by the firm belief of many neuroscientists.
This ‘corticocentric’ view of behavior has been used for diagnostic conclusions for so long without question. However, substantial evidence supports the hypothesis that brain-behavior associations goes far beyond the syndromes resulting from damage to the cortex.
White matter disease/dementia was a syndrome that came to light in neurological research in 1988, in order to highlight and further explain the relevance of white matter compared to gray matter and how cerebral white matter disorders produces cognitive loss of sufficient severity to qualify as dementia.
White matter disease may exist as a singularity disease at any age or as in some cases, may develop with other conditions associated with aging, such as stroke.
Multiple sclerosis and cerebral adrenoleukodystrophy may also result to white matter disease in young adult.
Types of White Matter Disease
There are numerous neurological disorders that professionals consider to be white matter diseases. Myelination is the formation of myelin sheaths (insulation layer) around nerve cells and the most common conditions considered as white matter disease are the impairment/abnormality to normal myelination or the damages to already fully myelinated nerve cells.
Damages affecting myelin can arise from either:
- Destruction of existing myelin (demyelinating diseases)
- Abnormalities in the formation of myelin (dysmyelinating diseases)
Processes that can cause the two above mentioned damages include genetic conditions, infections and autoimmune conditions.
Neuropathological summary of the categories of white matter disorder with carefully assigned examples include:
- Genetic (Metachromatic leukodystrophy)
- Metabolic (Vitamin B12 deficiency)
- Demyelinative (Multiple sclerosis)
- Vascular (Binswanger’s disease)
- Infections (HIV-associated dementia)
- Traumatic (traumatic brain injury)
- Inflammatory (systemic lupus erythematosus
- Neoplastic (Gilomatosis cerebri)
- Toxic (Toluene leukoencephalopathy)
- Hydrocephalic (normal pressure hydrocephalus)
In children, some forms of white matter disease such as dysmyelinating disease is very common. This is a form of white matter disease where the myelin does not form correctly; it can result from issues such as inherited enzyme deficiency.
Some examples of white matter disease in children include:
- Late infantile Metachromatic leukodystrophy: This condition occurs between 12 to 18 months after birth, the condition causes deterioration in speech, coordination and thinking skill in children. Children develop gait and posture problems within 2 years, as well as blindness and paralysis. It is typically fatal within 6 months to 4 years of symptoms onset but persons with the juvenile form of metachromatic leukodystrophy; which develops between age 4 and adolescence may live for years.
- Zellweger syndrome: This syndrome in children features liver dysfunction, jaundice, intellectual difficulties and irregular muscle tone. It leads to infant deaths and the severity of the condition varies.
- Vanishing WMD: Vanishing white matter disease is a very rare inherited condition that may develop during childhood. In this condition, early childhood onset of chronic neurological deterioration is mostly recorded.
- Krabbe disease: This is also known as ‘globoid cell leukodystrophy’, it can occur at any age but it common form is the infantile krabbe disease which starts before the first year. Krabbe disease causes increased muscle tone, fever, irritability and regression in development. This condition progresses rapidly and is fatal, mostly by the age of 2.
Prognosis on White Matter Disease
White matter disease comprises of different medical conditions that either be progressive, a form of the disease where individuals may notice their symptoms early, but the symptoms become worst as time goes on.
According to recent research and review of six large prospective studies, in persons suffering from white matter disease of unknown origin there is a higher risk of stroke and dementia compared to people without the disease.
The state of living expected for a person with white matter disease depends majorly on the specific type of white matter disease and the rate at which the disease progresses, not so much on the cause and complications.
Causes of White Matter Disease
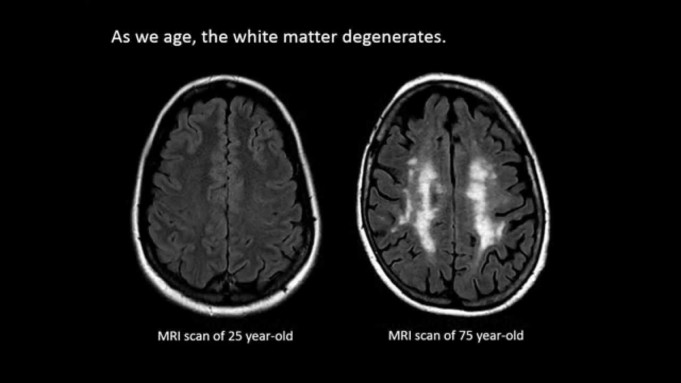
Most research pinpoint to the major cause of white matter degeneration to aging and presence of cardiovascular disease.
Although a study in 2014 suggests that the cause of white matter disease was unnoticeable strokes, strokes so small that it is unnoticeable to those having them.
The study referred to these strokes as “silent strokes”. These continuous silent strokes are believed to damage the white matter and cause white matter disease.
They also exist little evidence that white matter disease may be a cause of vascular dementia, however, there is no confirmative research to support this notion.
Many other conditions like disease, injuries and toxins can also cause changes in the nature of the white matter of the brain. Medical professionals have linked this disease to persons who is suffering from diabetes, parkinson’s disease, high cholesterol, a history of stroke.
Also, genetics may play a role in causing white matter disease.
Risk Factor for White Matter Disease
The most common risk factor for white matter disease is age. Other factors that may increase the risk of damaging the white matter are:
- Heart disease
- Smoking
- Progressing blood vessel inflammation
- Long-term high blood pressure
Symptoms of White Matter Disease
White matter disease has so many symptoms ranging from neurologic abnormalities to locomotive impairments but most of these symptoms might not surface until the condition has become severe.
The symptoms are progressive, getting worst with time. The role of White matter is crucial in communication within the brain and interaction between the brain and the spinal cord.
Symptoms include:
- Cognitive slowing
- Executive dysfunction
- Sustained attention deficit
- Memory retrieval deficit
- Visuospatial impairment
- Psychiatric disorder
- Relatively preserved language
- Depression
- Leaking urine
- Balancing dysfunction
It is very necessary to note that white matter disease is different from Alzheimer’s disease. Although both have very similar symptoms, Alzheimer’s disease affects the brain gray matter.
Tests will however be conducted to confirm the particular disease.
Diagnosis of White Matter Disease
Doctors begin diagnosis of white matter disease by examining medical history and presented symptoms, advance medical imaging of the brain may also be used.
Patients with white matter disease visit health professionals when they experience cognitive disorder and short-term memory losses. After physical examinations and investigations, an MRI test will likely be conducted.
A Magnetic Resonance Imaging (MRI) is a painless, noninvasive test that produces detailed images of the brain and the brain stream using magnetic resonance.
To view the white matter of the brain, the doctor has to use a specific type of MRI called T2 Flair. This type of MRI testing reveals details of the white matter in the brain, as well as revealing any abnormalities within the white matter.
Abnormalities in the white matter may appear as spots that are brighter than their surroundings. Doctors conclude diagnosis from the amount of the abnormal bright spots and the location of these spots.
A final diagnosis is made after the supervising doctor considers the MRI scan, cardiovascular health status result and symptoms presented.
Complications of White Matter Disease
The adventitious circumstances or conditions that might coexist or modify the existence of white matter disease come from the symptoms.
Some potential complications of white matter disease include:
- Strokes
- Balance issues and mobility limitations
- Vascular dementia
- Cognitive difficulties
Treatment of White Matter Disease
There is no direct treatment for white matter abnormalities, but health care professionals try to treat the underlying cause of the myelin degeneration or defect in hopes of slowing down the progression of the disease.
In cases of white matter disease due to small strokes, treatment options entail improving the cardiovascular health of the patient by eating a healthful diet, taking medications for hypertension or high cholesterol, and avoiding tobacco.
Multiple Sclerosis or progressive multifocal leukoencephalopathy which is a specific form of white matter disease may require other treatments.
Physical therapists will provide exercises and other physical therapy techniques to help patients with issues of balancing and locomotion limitations due to white matter disease to improve balance and gait.
Walking aids may be temporarily recommended.
Prevention of White Matter Disease
As we know, white matter disease related to age is progressive, that is, it gets worse with time. But steps can be taken to slow down its progression rate.
Clinicians believe that damages to the white matter can be undone if attended to early. Other tips to prevent the occurrence of white matter disease include keeping blood pressure and blood sugar in check, keeping the health healthy, follow a low-fat low-salt diet, and moderately intense exercises once a while.
Also, Diabetics are advised to manage their conditions well, keep cholesterol in check and quit smoking.
Summary
White matter disease is a condition of the brain that is mostly related to myelin. The condition opened medical professionals to the relevance of the white matter and its contribution to cognitive functions.
White matter disease is progressive and mostly occurs in elderly individuals, although, it has been discovered in its infantile form, occurring in children, if diagnosed early enough, the rate of progression can be reduced and medical tips on how to combat its symptoms are also available.
Sources
- White Matter Disease; http://www.ahajournals.org/doi/10.1161/STROKEAHA.120.032148
- Vanishing white matter disease; https://www.sciencedirect.com/topics/medicine-and-dentistry/white-matter-disease
- White matter dementia; http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3437529/
- Leukoaraiosis; https://en.m.wikipedia.org/wiki/Leukoaraiosis