Neglected tropical diseases (NTDs) are a diverse group of infections that mainly impacts impoverished areas in tropical regions around the world. NTDs are Found in 149 countries and have address more than a billion people so far.
NTDs affect more individuals than common illnesses like tuberculosis, malaria, and HIV combined throughout the worldwide and lead to nearly 57 million years of life lost when you consider the disability and premature deaths they cause.
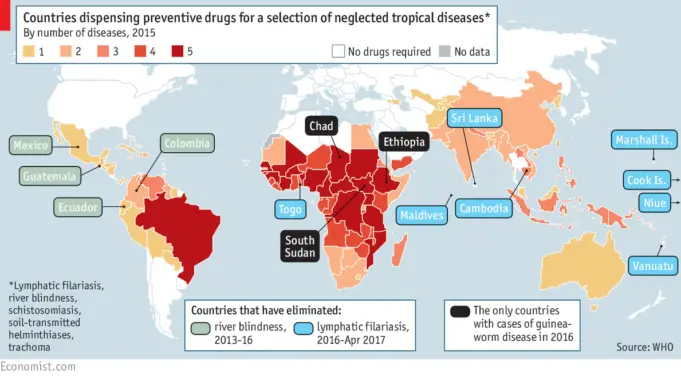
Many of these Neglected tropical diseases are easily preventable with low-cost meds; however, logistical and economic problems of the places where these infections exist to make it challenging to combat them.
Even so, the effects of NTDs has gained increasing attention in recent times, and much progress has been made when it comes to eliminating a good number of these infections.
Examples of NTDs
In June 2018, the World Health Organization was able to list at least 21 conditions and infections as NTDs, many of which no longer exist in developing countries at the moment but can still be found in the world’s most underdeveloped and impoverished areas.
These diseases can only thrive in the absence of safe drinking water, medical care, or adequate sanitation, yet a significant number of them are treatable for as low as 50 cents per individual, per year.
The WHO, together with organizations such as UNICEF and the Centers for Disease Control and Prevention (CDC) have made efforts to draw more attention to NTDs, in an attempt to garner increased political will and resources to tackle them; nevertheless, these infections still affect at least one in six people worldwide.
The first significant breakthrough for combatting NTDs occurred in 2007 when a group of almost 200 people from different public and private organizations from different parts of the globe came together at the headquarters of WHO in Switzerland to talk about how the world can collaborate to combat these diseases.
Since that time, the WHO and its many partners have established plans to reduce or eradicate NTDs, pleading those in wealthier parts of the world to pitch in.
NTDs can roughly be broken down into four categories: viruses, helminths (worms or worm-like organisms), bacteria, and protozoa (parasites).
NTDs are spread through insects and animals, from person to person, or by coming in contact with, or consuming contaminated water or food sources. The list of NTDs that have been identified by the WHO as of June 2018 includes:
- Chagas disease
- Buruli ulcer
- Dengue
- Chikungunya
- Echinococcosis
- Dracunculiasis (guinea worm disease)
- Human African trypanosomiasis (African sleeping sickness)
- Foodborne trematodes
- Leprosy (Hansen’s disease)
- Leishmaniasis
- Lymphatic filariasis
- Onchocerciasis (river blindness)
- Mycetoma, chromoblastomycosis, and other deep mycoses
- Rabies
- Schistosomiasis (snail fever)
- Scabies and other ectoparasites
- Snakebite envenoming
- Soil-transmitted helminthiases
- Trachoma
- Taeniasis/Cysticercosis
- Yaws (Endemic treponematoses)
Who gets affected by NTDs
Regardless of their diversity, all NTDs have one link in common: they disproportionately impact people who are living in poverty. Many remote areas around the world still do not have proper access to clean water, basic sanitation, and modern medical care.
Typically (except in rare cases), these infections can be found in tropical areas, especially in communities where people live around livestock, animals, or insects that carry and transmit the parasites and pathogens.
The huge impact that NTDs have on the world is jaw-dropping. More than one billion people around the world are currently infected with one NTD or another (many people have more than one at a time), and over half the world’s population reside in areas where there is a risk of getting an NTD infection.
An estimated 185,000 people may die each year as a result of dealing with at least one NTD, and millions of others live with chronic infectious diseases.
When people can survive them, NTDs can prove to be debilitating, causing long-term health problems, personal and financial difficulties, and physical pains or suffering.
They prevent people from working like they should or even learning, perpetuating, and increasing a cycle of poverty in the poorest of the poor populations around the world.
On an individual level, this can trigger financial difficulty, but amplified across several communities and countries where these illnesses are common; it can also be economically draining.
According to an estimate, nations where lymphatic filariasis (elephantiasis) exist lose $1 billion yearly and as much as 88% of their economic activity because of that singular disease alone.
In addition to the impact that NTDs has on the physical health of infected people, research shows that it can affect their mental health, as well as on psychological development, also.
Children who have early and regular parasitic infections are at a higher risk for anemia and malnutrition, which can significantly
or even irreversibly affect their cognitive and learning abilities.
Adults become permanently disabled or disfigured as a result of an NTD infection, and they often have to face stigma, discrimination, or even exclusion from employment opportunities, educational institutions, or the society in general. This is something that can significantly affect their mental health.
While it is true that most NTDs hit developing nations the hardest, poor people who live in wealthy nations are not immune to NTDs. This means that poor people in countries like the United States can also be affected.
Southern states located along the Gulf Coast and Mexico border that have high recorded poverty rates are especially vulnerable, so too are U.S. territories such as Puerto Rico.
Researchers have estimates nearly 37,000 current reported cases of Chagas disease in Texas alone, for instance, with over 200,000 believed to be spotted throughout the other parts of the United States.
There have also been reported outbreaks of mosquito-borne NTDs such as dengue virus and chikungunya in the country and its territories. Some researchers have also pointed out that cases may become more frequent with the rise in global temperatures, and the frequency in international travels.
Challenges
Naming these diseases “neglected” was not a coincidence nor an accident. Many government bodies overlook NTDs, and so do public health agencies, and even research institutions in wealthy nations as these diseases do not typically affect their population.
Unfortunately, the countries that usually report NTDs are those that are poor and unable to fight the diseases by themselves.
International coalitions spearheaded by the WHO have achieved some progress in recruiting more wealthy countries and global partners to get rid of NTDs, but it’s an uphill because of a lack of resources, information, and coordination.
Lack of Information
The first step to combating any kind of disease is to have a clear understanding of them: where they are dominant, who they impact, what the most effective treatment is, etc.
But since NTD outbreaks are recorded mostly in low-income and usually rural or remote communities, the health officials on the ground frequently do not possess the tools they require to spot or effectively report the diseases.
However, without that information, it can be challenging for international organizations to transfer the right materials for treatment to the right places.
Lack of Resources
Each unique NTD requires a specific strategy to combat or control it. While some may need serious medication distribution programs, many others require vector control (such as mosquito spraying), and some need a combination of the two.
For their role, many pharmaceutical companies have donated large amounts of medications for the treatment of NTDs. However, it takes significant resources to get drugs to the affected communities. There is also the problem of vehicles or fuel to arrive at the remote areas and medical hands to administer them.
For those infections that have no effective treatment or prevention methods, developing new vaccines or medications is quite expensive and challenging that few companies or organizations will even try to take it on.
Lack of Coordination
Worms, parasites, viruses, and bacteria do not confine themselves to any boundaries of geopolitical borders, but usually, efforts towards disease control are conducted in that manner.
More power and fixes can be done with fewer resources when government and organizations pool their assets and knowledge to collaborate on subjects like distributing medications or controlling insect populations in affected areas.
This coordination is one that requires active involvement by people from both wealthy nations who are willing to lend a helping hand and those on the ground in places that are most impacted by NTDs.
The WHO is working with a wide variety of governments and organizations, but directing and juggling all the players—each with their own needs and agendas can be like trying to herd cats.
Also, acquiring and distributing the correct materials to those who need them the most can be tough to do in places where the local leaders are not interested in any form of help from outsiders.
Lack of Political Will
To eliminate NTDs on a global scale will require a considerable amount of resources and energy, which also requires so much political will.
Those who are in power —governments, billionaires, international nonprofit organizations, and philanthropic corporations also need to get involved, if there must be enough resources or momentum for making headway.
There has been a significant increase in interest to combat NTDs from all around the world, both from wealthy nations and nonprofits (such as the Carter Center). However, so much more is required.
To increase political will, more constituents in wealthy countries will need to call out to their elected officials to plead with them to both support funding for and actively participate in programs for the NTD elimination.
WHO Recommended Solutions
Considering the scale, diversity, and the logistical challenges that save to do with combatting NTDs, fighting them may an m challenging one, but it is not an impossible one.
The WHO has recommended five strategies for tackling NTDs, many of which will require massive investments and coordination from both private, public, and academic partners in different countries from all over the world.
Therapies, and preventive Treatments
In cases where there already is an effective single-dose treatment, the WHO goes further to advocates large-scale programs to preemptively offer these medications to populations who are at risk for infections frequently as a complement to other strategies, like improved sanitation.
Instead of waiting for each person to be diagnosed and treated in a fully equipped medical setting.
These programs require the aid of volunteers and other non-specialized personnel, instead of nurses in a clinic, to offer the medication in non-clinical settings, for instance, giving school children in southern Rwanda a drug for the treatment of soil-based helminths.
Innovation in Disease Management
Many NTDs are challenging to diagnose or even detect, difficult to treat, and do not have effective prevention strategies such as vaccines.
To tackle NTDs in a meaningful manner, health officials and researchers will have to modify or develop techniques to be better suited to the areas where NTDs have been located.
Other strategies include:
- Vector Control
- Basic Sanitation
- Control of Zoonotic Diseases
NTDs are still being tackled around the globe, and excellent results have been recorded in some areas.
However, individuals also have a role to play in controlling the spread of such diseases, and even in eliminating them from poor or remote areas. We hope that you found this article helpful. Please leave a comment below.