The name ‘bright disease’ is a historical term that refers to a disease, the name is no longer in use; this disease involves the inflammation of the internal structures of the kidneys- glomeruli, which are made up of tiny blood vessels.
Currently, the disease is medically termed glomerulonephritis (GN) or chronic nephritis (CN), but for convenience, we are going to be using the historical term- bright disease.
The Human Kidney
In order to fully understand the relevance of bright disease, we are going to need an abstract view of the kidney.
The kidney is the major excretory and osmoregulatory organ of mammals and its functions include Removal of metabolic waste products, regulation of the water content of the body fluids, regulation of the pH of the body fluids, and regulation of the chemical composition of the body fluids by removal of substances which are in excess of immediate requirements. The kidney has a rich blood supply and regulates the blood composition at a steady state.
There is a pair of kidneys in humans situated towards the back of the lower part of the abdominal cavity, on either side of the vertebral column with the left kidney slightly above the right kidney in positioning.
A traverse section of the kidney shows two distinct regions; an outer cortex and an inner medulla. The cortex is covered by fibrous connective tissues, forming a tough capsule.
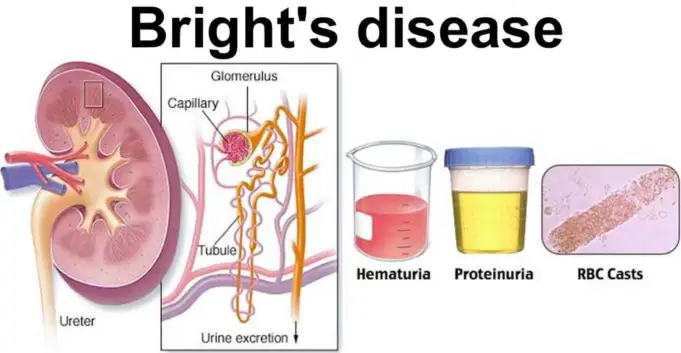
The cortex of the kidney contains glomeruli, which is visible with the naked eyes, renal capsules, and parts of the nephrons. The medulla is composed of tubular parts of the nephron and blood vessels, which together form renal pyramids.
The normal aging process of an individual affects kidney function in various ways, particularly the efficiency of the filtering process, this gradual decline is about 50% by age 70. Some people, however, experience kidney disease, which is abnormal kidney functioning.
A general term for a decline in kidney performance as a result of the disease is kidney failure. Kidney disease is a relatively common disease, affecting people in their tens of thousands all over the world. It may be chronic or acute. Chronic kidney failure is progressive and takes place over a number of years.
Acute kidney failure on the other hand is when the kidney function stops or almost completely stops, relatively suddenly. If kidney failure is not treated, death will result within a couple of weeks, often due to the buildup of potassium ions which causes heart failure.
If one kidney fails, it is possible to live but if both fail medical intervention is vital.
History of Bright disease
Bright disease or glomerulonephritis (GN) is a chronic kidney disease, its symptoms were first to mention in 1827 by Richard Bright.
In his medical cases reported, he described 25 patient cases involving dropsy (which is now termed edema; an excessive accumulation of serum in tissue spaces or a body cavity) and linked each of these cases to kidney failure.
Following the initial report of Richard Bright, subsequent researches conducted revealed a connection between heart hypertrophy (an increase in the size of the heart) and kidney disease, birthing a hypothesis that stimulation of the heart was involved in Bright’s medical discovery.
One remarkable case of Bright’s disease at that time was the case of Arnold Ehret; his condition was diagnosed as incurable by 24 expert and respected physicians in Europe, however, he eventually cured himself of the disease with the design of ‘The Mucusless Diet Healing System’. In recent times and in modern medicine, the name ‘Bright’s disease’ is no longer used and only serves as a reference for historical purposes.
The reason is that Bright’s disease was an umbrella term due to a vast range of renal diseases for which now have more precisely descriptive terms in modern medicine. But the complexity of the syndromes that Richard Bright disclosed in his medical reports led later to the reclassification under the term glomerulonephritis or nephritis.
Causes of Bright ’s Disease
The bright disease involves the inflammation of the blood vessels and other structures of the kidney. These knots of blood vessels and glomeruli helps filter and remove excess fluids and chemical composition in the blood.
If the glomeruli of the kidney are damaged, the kidney will stop functioning normally, leading to kidney failure. Bright’s disease can be life-threatening as the causes of the disease can either lead to an acute (suddenly) or chronic (long term).
Acute Bright’s Disease is usually due to a response to an infection such as abscess tooth (when a bacterial infection causes the tooth to be filled with pus and other infected materials) or strep throat (a bacterial infection that causes inflammation and pain in the throat).
Acute Bright’s disease may also be due to immune system dysfunction; like overreaction of the immune system to an infection.
Acute Bright’s disease is characterized by severe inflammation, swelling, increased blood pressure, renal insufficiency, and severe back pain. These conditions can be adequately treated but if the body does not respond positively to the treatments then prompt medical attention to prevent long-term damages to the kidneys.
Some other ailments that can also cause acute Bright’s disease (glomerulonephritis GN), include;
- Systemic lupus erythematosus: commonly known as lupus (an autoimmune condition).
- Amyloidosis: occurs when an abnormal protein that can cause harm builds up in the kidney and other tissues.
- Goodpasture syndrome: an autoimmune condition where antibodies produced by the immune system begins to attack the cells of the lungs and kidney; It is very rare.
- Polyarteritis nodosa: this a serious disease of the blood vessels characterized by swollen arteries (especially the arteries) caused by an immune system malfunction. When the arteries of the kidney are affected, it causes acute glomerulonephritis.
- Hypertension: high blood pressure can cause damage to the glomeruli.
Risk factor of Acute Bright’s Disease
Heavy medication use of non-steroidal anti-inflammatory drugs such as naproxen and ibuprofen can be a major risk factor for acute glomerulonephritis.
Abusing such medications for a lengthy period of time can damage the internal structures of the kidney.
Chronic Bright disease or glomerulonephritis is another form of Bright’s disease that evolves over several years; it can pose very few symptoms, or it can be completely asymptomatic.
These progressive developments of chronic glomerulonephritis cause permanent damages to the kidney and its structures and ultimately lead to complete shutting down of the kidney.
The etiology of the origin of this form of Bright’s disease is usually unclear. It can be a secondary function of a genetic disease, as hereditary nephritis has been reported in young males with poor vision and hearing.
Other speculated causes include:
- A history case of cancer
- Exposure to some hydrocarbon
- Certain immune disease
- Heart and liver problems
- Diabetes
Stages of Bright’s Disease
Bright’s disease as seen in some cases and other kidney failure cases can be classified into stages, taking different forms from Acute form/stage to Sub-acute form and finally a chronic form later on over a period of years.
Acute Bright’s disease recovery is usually fairly completed after an episode, but minor infections may do further damage to the kidneys and their structures and bring on the sub-acute and chronic stages.
The Sub-acute stage of Bright’s disease does not necessarily follow acute attacks, however, if it does develop, it usually follows the acute stage several months or years after.
The kidney becomes larger and it surface becomes smooth and pale, while the internal tissue is darker than usual. The paleness of the kidney in this stage is due to the restriction in blood flow to the surface portion of the kidney and the high gathering of lipid (fat) droplets and the darker internal tissue is due to degeneration of the nephron tubules.
Because of the breakdown of kidney tissues, a larger amount of blood protein than usual is released into the urine. Red blood cells forced through the constricted glomeruli become crushed, distorted, and fragmented; the loss of red blood cells leads to anemia.
In the last stage of a kidney failure- chronic Bright’s disease, the kidney is reduced mostly to scar tissue. It becomes small and shriveled and its surface is granular.
Because filtration of the blood can no longer occur because of the bad condition of the kidney, levels of abnormal quantities of nitrogenous substances and other waste product increases aggressively in the blood which lead to a condition called uremia.
Symptoms of Bright Disease
Generally, symptoms of kidney failure include fatigue, loss of appetite, insomnia, dry and itchy skin, muscle cramps at night, nausea and vomiting.
According to the types and stages of Bright’s disease, the severity of these symptoms may vary, these specific stages according to the forms of Bright’s disease include:
Acute Bright Disease
Symptoms in this category have early onset, they include:
- High blood pressure
- Puffiness in your face
- Less Urinating frequencies
- Extra fluid in the lungs (Edema)
- Coughing
- Apoplexy, cerebral hemorrhage resulting ion stroke.
- Convulsion
Chronic Bright Disease
A chronic form of Bright’s disease can occur without caution as many cases are reported to be asymptomatic. Other cases are slow development of symptoms similar to the acute form. Some symptoms include:
- Albumin (excess protein) in the urine which show up during a urinalysis test.
- High blood pressure
- Swelling of the face and joints due to accumulation of fluid.
- Frequent nighttime urination
- Abdominal and back pains
- comma
- Frequent nosebleeds
- Vision impairments
- Inflammation of serous membranes
- Hemorrhages
- Protrusion and discoloration of veins especially in the legs
Diagnosis of Bright’s Disease
In the diagnosis of Bright’s disease, the initiative step is a urinalysis test (urine test). Blood and protein in urine are very important markers for inflammation of the glomeruli and nephron.
Other medical and physical examinations for other clinical conditions can also lead to the discovery of glomerulonephritis (Bright’s disease).
More than one urine is necessary to check significantly the health state of the kidneys, such test reveals:
- Creatinine clearance
- Urine concentration
- Urine specific gravity
- Urine red blood cells
- Urine osmolality and osmolarity
- Total amount of protein in urine
Blood tests are also conducted to show:
- Abnormal albumin levels
- Anemia, which is a low level of red blood cells.
- Creatinine levels
- Abnormal blood urea nitrogen
Immunology tests are also recommended by specialists to show if the immune system is attacking the kidneys, the tests checks for:
- Antinuclear antibodies
- Antiglomerular basement membrane antibodies
- Complement levels.
- Antineutrophil cytoplasmic antibodies
In some other cases, tissue biopsy of the kidney is carried out to confirm diagnosis; this involve analyzing a small, collected sample of the kidney tissues, the sample is collected by a needle.
Other imaging tests are also carried out, such as CT scan, Chest X-ray, intravenous pyelogram and kidney ultrasound scan.
Treatment of Bright’s Disease
In old times, the traditional treatments of Bright’s disease included a wide range of techniques such as:
- Warm baths
- Blood letting
- Herbs with diuretic properties
- Squill
- Opium
- Mercury
- Avoidance of alcohol, cheese and meat
- Laxatives
The efficacy of these treatment techniques varied considerably between each case and the involved factors. This is however expected as the term ‘Bright’s Disease’ was an umbrella term for a variety of wide conditions linking to the kidney based on their shared symptoms.
Today, the treatment method varies depending on the type of Bright’s disease and its etiology.
An example of a treatment approach is the control of high blood pressure, especially if that is the underlying cause of the glomerulonephritis. Blood pressure may be very hard to control when the kidney(s) are not functioning properly.
This becoming the case, the doctor may prescribe blood pressure drugs including ACE (angiotensin-converting enzyme) inhibitors, such as; lisinopril, captopril, peridopril. Angiotensin receptors blocker (ARBs) medications may also be prescribed, like; losartan, valsartan and Irbedartan.
Another treatment approach is to reduce immune triggered inflammations; an arm of this treatment can be the use of Corticosteroids to reduce immune response, or plasmapheresis– a process that involves removing the fluid part of the blood (plasma) and replacing it with intravenous fluids or donated plasma that contains no antibodies.
For cases of chronic Bright’s disease in treatment and also as a preventive measure, the amount of diet protein, salt and potassium in recommended to be reduced. Additionally, liquid contents must be cautioned (like alcohol).
Calcium supplements are recommended, and in cases of swelling, patient may require diuretics (medication that increases the amount of frequency of urination) from a medical dietician.
In a worst-case scenario if Bright’s disease advances in a kidney failure, the patient mat need to have a dialysis; a procedure where a medical machine filters the blood and eventually, a kidney transplant may be needed.
Complications of Bright’s Disease
Bright disease may lead to other dangerous medical conditions which are medically termed ‘Complications of GN’. The following complications include:
- Chronic urinary tract infection
- Acute kidney failure
- Congestive heart failure due to retained fluid or fluid overload.
- Acute kidney failure
- Chronic kidney disease
- Pulmonary edema due to retained fluid or fluid overload.
- High blood pressure
- Malignant hypertension, which is a rapidly increasing high blood pressure condition.
- Increased risk of infection
- Electrolyte imbalance and so on
Summary
If Bright’s Disease is diagnosed and attended to early, acute Bright’s disease can be temporary and very reversible. Chronic Bright disease may be slow with early treatment, but progress can be recorded.
The following steps have shown positive impact in recovering from Bright’s disease (glomerulonephritis) and preventing future occurrence:
- Maintain a healthy weight.
- Restrict protein in your diet.
- Restrict potassium in your diet.
- Quit smoking and alcohol.
- Restrict salt in diet.
In addition, meeting with a support group(s) can be a helpful way for you to deal with the emotional stress of having a kidney disease.
Sources;
- History of Bright’s Disease; http://jamanetwork.com/Journals/jama/article-abstract/297842
- Treatment; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1786202/
- Chronic Bright’s disease; https://www.sciencedirect.com/topics/medicine-and-dentistry/brights-disease
- Bright Disease; https://www.britannica.com/science/Bright-disease