Reactive airway disease is an umbrella term used controversially by medical professionals to describe a group of symptoms that may or may not be caused by asthma.
Most times, Reactive airway disease and asthma are used interchangeably. However, there are some significant differences between the two.
The term “reactive airway disease” does not give a clear or pinpoint to a definite disorder or disease and it may be used to report different conditions.
Individuals suffering from reactive airway disease have bronchial tubes that overreact to some particular foreign particles or irritants.
In this condition, people are mostly observed to wheeze and sometimes experience bronchial spasm, this sensitivity response is mostly seen in people who are asthmatic or suffer from chronic obstructive pulmonary disease (COPD), emphysema, or a viral upper respiratory illness, but medical histories of reactive airway disease patient mostly don’t show any diagnosis of these airway disorders.
There are so many medical controversies over the use of reactive airway disease as a label in the healthcare setting, often due to the equivoque definition that the term has.
Also, Reactive airway disease can be mistaken for reactive airways dysfunction syndrome; an asthma-like disease that is caused by high exposure to vapors, fumes, and secondhand smoke.
Unlike reactive airway disease, with which physicians are still struggling in the applicative use of the term, Reactive airways dysfunction syndrome has been approved and is recognized by multiple medical societies as a real clinical syndrome, such as America Thoracic Society and America College of Chest Physicians.
The use of the term ‘reactive airway disease’ originally began to appear in the 1980s in a published medical literature which was in reference to asthmatic patients with hyperactive bronchial tracts.
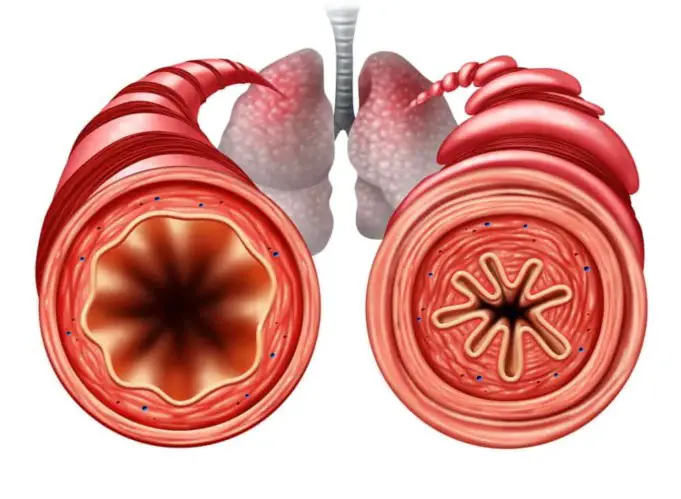
This over-reactivity of the bronchial (mostly increased bronchoconstriction reaction) is a common symptom of asthma which entails a response to stimuli that shouldn’t evoke such a response.
However, after the introduction of this term, it soon became familiar with description and suddenly began to be used interchangeably with asthma.
A 2001 published medical paper explained the use of the term as having “no clinical meaning” and an “annoyance” to doctors seeking “diagnostic clarity”. Most recently, clinicians commonly use the term reactive airway disease when they are hesitant to conclude a patient is asthmatic or has its symptoms.
Causes of Reactive Airway Disease (RAD)
Reactive airway disease is very similar to asthma, and like asthma it occurs mostly after an episode of infection.
This infection may have triggered a severe inflammation of the bronchial and even when the infection is past, there is an autoimmune reaction of the bronchial and the bronchioles to any particle or irritant, which results in swelling.
This swelling causes the airway to become narrow making it difficult to breathe. Most irritants that trigger this reaction may include the following, with most working in combination with others:
- Pollens
- Perfume
- Smoke
- Dust
- Distilled water
- Mildew
- Hair particles
- Change in weather.
- Stress
- Exercise
- Other strong odors
Risk factors of Reactive Airway Disease (RAD)
The category of individuals that are most at risk of developing this disorder are lifelong cigarette smokers, standing at a 50% chance of developing RAD. Smoking irritates the airways and also damages the lungs
Continually irritating the airways by smoking increases the risk of chronic obstructive pulmonary disease (COPD) developing later; COPD is incurable.
Also, other factors may increase the chances of reactive airway disease, including:
- Family history of reactive airway disease (rarely)
- Occupational exposure to chemicals smoke and fumes such as Firefighters, police and other emergency services workers, cleaners, welders, and farmers.
Symptoms of Reactive Airway Disease (RAD)
The symptoms of reactive airway disease are the same as those seen in asthma. These symptoms are indications that the airways have been irritated and they include the following:
- Breathing difficulty
- Feeling of tightness in the chest
- Mucus in the airways
- Wheezing
- Coughing
- Swelling of the lining of the airways
- Hypersensitive bronchial tubes
- Shortness of breath
Diagnosis of Reactive Airway Disease (RAD)
Reactive airway disease is mostly diagnosed the same way as asthma and most reactive airway diagnostic are resulting cases of other airway disorders.
If an individual mostly children is exhibiting asthmatic signs but may be too young to have diagnostic testing to confirm that diagnosis, and health care provider may diagnose the child with reactive airway disease:
- Skin testing: This is known as a scratch test; skin testing exposes the skin to small amounts of allergens (allergy-causing substances) and can identify allergy triggers, such as pollen, dust, mites, pets, or mold that may be causing reactive airway disease.
- Pulmonary (lung) function tests: This is a noninvasive lung function test that provides information on how well the lungs are working. Children younger than 5 years may be too young for this testing, so the test is mostly performed in older children and adults with reactive airway disease to confirm the diagnosis. There are several types of pulmonary function tests:
- Spirometry: A spirometry test is a lab test that measures the amount of air the lungs can hold, and the amount can be forcefully breathed out. In the case of reactive airway disease condition, the amount of air is very low compared to values from a normal lung or airway.
- Lung volume test: This is a type of pulmonary test that measures the volume of air in the lungs and the amount that is left in the lungs after a complete breath.
Further testing may be conducted to look out for other conditions that affect the pulmonary system such as pneumonia, virus infection, or emphysema.
Medications and Treatment

After the first round of diagnosis for reactive airway disease is conducted, to ease symptoms, and health care provider may introduce an inhaler medication also known as a bronchodilator for the meantime and recommend further tests to be later conducted.
The results post-bronchodilator use is compared to the results before the introduction of an inhaler, to confirm the effectiveness of the medication.
Medication helps to treat reactive airway disease or underlying health conditions that may be causing it. Some asthma medications are administered to provide swift relief from reactive airway disease symptoms and other medications are administered daily for long-term symptom control.
If the condition is allergy-related, allergy medications will be of great help. Information on medications suitable against a particular airway disease should be always provided by a doctor.
Other treatment techniques used against reactive airway diseases depending on the cause and the severity of the reaction to these triggers, include the use of breathing and relaxation exercises for a stress-triggered RAD, treating an infection for viral triggered reaction, and use of a rescue inhaler or ventilator also effective for an exercise or stress-induced reaction.
Conclusion
Although it seems totally impossible to prevent reactive airway disease, there are few steps one can take to prevent flare-ups. Also, people can avoid reactive airway disease triggers and follow doctor instructions for medication usage.
People should immediately visit a doctor when they experience breathing difficulties without a known reason as he/she may be experiencing reactive airway disease symptoms.
If also an individual is experiencing shortness of breath and is to undergo surgery for any other reason, the medical team to conduct the surgery should be duly informed about the breathing troubles
In this case, the anesthesiologist will provide accommodations and take precautions. In young children with reactive airway disease, it is very important to confirm if the condition is asthma or not, the revelation will ensure proper treatment and prevent dangerous asthmatic attacks in near future.
Sources;
- Reactive airway disease; www.atsjournals.org/doi/full/10.1164/ajrccm.163.4.2005049
- Reactive airway disease (Adult); http://www.lahey.org/lhmc/department/allergy-and-immunology/conditions-diagnosis/reactive-airway-disease-adult/
- RAD; http://pediatrics.aappublications.org/content/139/1/e20160625