The gut-brain axis is simply a biochemical signaling that occurs between the central nervous system (CNS) and the gastrointestinal tracts (GI tract). Your gut flora plays a great role in this communication.
The gut-brain axis involves a lot of systems and processes in the body. This post will help you understand how the gut and brain communicate with each other and affect your overall health.
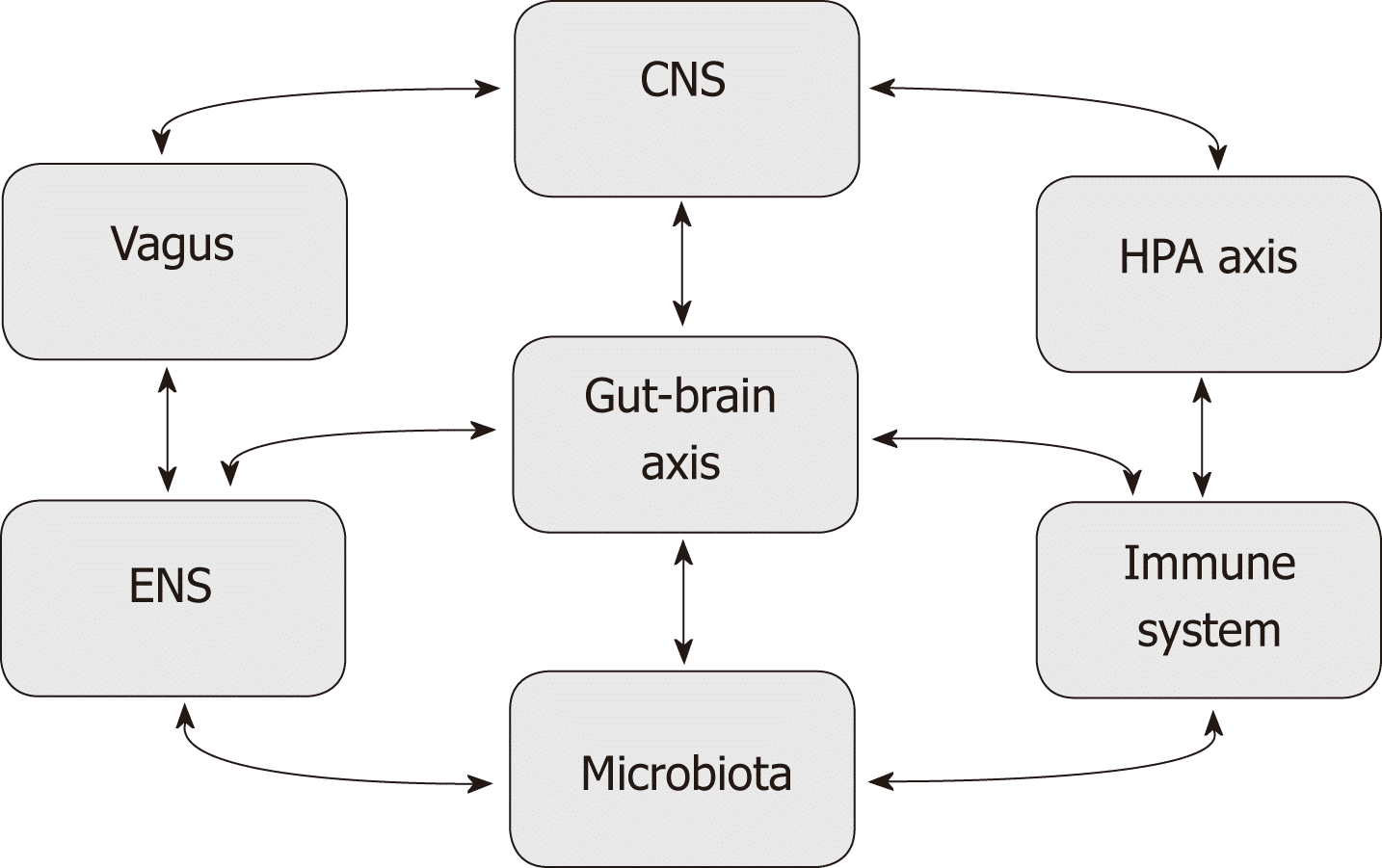
There are direct and indirect pathways between the emotional and cognitive centers of the brain and the functions of your peripheral intestinal functions.
There are also complex processes between the gut and the endocrine, immune, and autonomic nervous systems. This makes it possible for the gut-brain axis to drive efferent and afferent neural signals between the brain and the gut.
This system gives the brain influence on intestinal functions which include the immune, epithelial, and smooth muscle cells. It also includes enteric neurons.
Understanding the Gut and the Microbiome
The population of microbes and their genetic material in the gut is known as the microbiome. This has an influence on your gastrointestinal tract. Recent studies are letting us know that the microbiome plays an important role in the structure of the gut-brain axis and your overall health.
Many confuse microbiome and microbiota. Microbiota is the population of microbes on a specific ecosystem such as skin or gut. An example is the skin microbiota or gut microbiota.
There are trillions of microbes in your gut, they are 10 times more than all the cells in your body. The whole genetic material of your microbiome is 150 times more than your human genome.
This is why some scientists call it a “superorganism”. They play unique roles in health and diseases. A disruption to the population and balance of this microbiome will cause autoimmune diseases, allergies, neuropsychiatric disorders, and metabolic disorders.
It can also cause digestive issues like irritable bowel syndrome (IBS), depression, autism, obesity, anxiety, autism, and many more.
These conditions are plaguing the world today. Your gut makes up to 70 to 80% of your immune system. It is known as the largest immune organ in the body. Your gut is also regarded as your second brain.
It is sensitive to emotions. All kinds of emotions can trigger symptoms in the gut. That’s why some experience can give you butterflies in your stomach while some can make you feel nauseous.
The brain has a direct effect on your gastrointestinal tract and vice versa. That is why the thought of eating can release digestive juices even before you eat. A troubled brain can send signals to the intestines just as a troubled intestine can send signals to the brain.
This is why stress and emotions are considered when treating gastrointestinal disorders and a distressed gut.
The Gut-Brain Axis and Why it Matters
At birth, a newborn baby is exposed to the vaginal microbiota of the mother. This will influence the creation of microbiome in the baby. The gut microbiota is the foundation for the development of the central nervous system and enteric nervous system in the early weeks after birth.
The interaction between the gut microbiome and the mucosal lining will help the development of the immune system. The gut microbiome will produce healthy levels of neurotransmitters which help improve health and play great roles in diseases.
The vagus nerve, which is the largest nerve in the body, connects the gut and the brain. This is their medium of communication. Other pathways are also involved in this complex connection.
Some are through the endocrine system, some are through various chemical messengers, neurotransmitters, and gut hormones. Most of these neurotransmitters and hormones are made in the gut.
Some of the neurochemicals and hormones produced in the gut are GABA, serotonin, dopamine, and short-chain fatty acids. This simply shows why the activities going on in the gut can affect your brain and mental health.
Roles the Gut-Brain Axis Play in Diseases
Digestive Disorders
Changes in the population of microbiome and the communication between the brain and the gut can lead to digestive problems like IBS. This can be induced by excess stress.
When under chronic stress, the fight-or-flight response of the body is activated. This is the normal reaction of your body in response to danger or threat.
When this is activated, digestion is slowed down because the body wants to use its whole energy to deal with the danger at hand. This, in turn, will increase gut sensitivity.
This will lead to the symptoms of IBS which includes bloating, altered bowel movement, flatulence, stomach pain, etc. When under constant stress, your body feels like you are running from danger and this will affect your gut-brain axis.
Another way your gut can affect your health is through the presence of visceral hypersensitivity. This is high perception of pain around your gut. This can alter the functions of your gut and lead to the symptoms of IBS like stomach pain and bloating.
This is caused by an over-active response from the gut to the brain. This leads to a heightened or exaggerated perception of pain. Even studies have shown that there is a difference in the microbiome of people with IBS.
There is usually an imbalance in the community of microbes. Both the numbers and diversity of the microbes are affected and they can change and become potentially harmful. This is known as gut dysbiosis.
Stress can alter your gut microbiome. It makes IBS worse, reduces the population of healthy bacteria like the lactobacillus, and change the profile of your gut community.
Inflammation
Your immune system also connects your gut-brain axis. Your gut microbiome plays an important role in inflammation and your immune system by controlling what goes into your bloodstream and what is excreted.
Inflammation can occur if your immune system is switched on for too long. This can trigger Alzheimer’s disease and depression. Lipopolysaccharide is a toxin that causes inflammation and it is produced by microbes in the gut.
Inflammation can occur if an excess of this toxin passes into the bloodstream from your gut. A compromised or leaky barrier can cause this. This can even lead to dementia and schizophrenia.
Also, remember that inflammation is the root cause of most chronic diseases like diabetes.
Anxiety and depression
The microbiota in your gut regulates the functions of your brain and behavior. The gut microbiota is involved in many psychiatric disorders like anxiety, depression, and even mental problems.
People who suffer from the above mental problems have differences in their gut microbiome. This is the trigger of mental health conditions. People who suffer from depression have a reduced population of healthy microbes in their gut.
Production of chemicals
The gut produces chemicals that affect the brain. These include dopamine, serotonin, acetate, propionate, butyrate, etc. these have a lot of functions on your mental and overall health.
Butyrate produced is used in forming the blood-brain barrier which protects the brain.
How to Improve your Gut Microbiome
The main way to improve the health and functions of your health microbiome is through diet. A healthy diet can improve your gut microbiome and boost your mental health.
A diet rich in fruits and vegetables, nuts, and seeds, whole-grains, legumes, and mostly a whole plant-based diet will improve the population of healthy microbes in your gut.
These foods will also increase the diversity of the healthy microbes present in your gut. A special class of food to include in your daily diet to boost your gut health is probiotics.
Probiotics are rich in healthy microbes, and ingesting them will improve your gut microbiome and affect your mental health positively.
Probiotics are gotten by fermenting healthy foods such as fruits vegetables, grains, and even organic dairy. You can find probiotics in fermented foods like sauerkraut, kefir, and yogurt.
They are also available in the form of supplements. They are many strains or probiotics and each has its own unique functions on the body. Prebiotics are simply the foods eaten by the probiotics in your gut.
They help them multiply and carry out their functions. Prebiotics are found in high-fiber foods, whole grains, garlic, onions, legumes, fruits, vegetables, nuts, etc.
They act as fuel for the healthy microbes in your gut. This will help them grow and thrive. Increasing your intake of prebiotics will have a direct influence on the gut-brain axis, and this, in turn, would boost your health, mood, and even behavior.
In boosting the health of your gut microbiome, you have to avoid foods and lifestyles that affect it. This includes processed foods, refined sugar, antibiotics, alcohol, excess fats, white flour, and unnatural food additives and colorings.
You also have to live an active lifestyle, sedentary living affects your gut microbiome, and indirectly your mental and overall health. You also have to reduce your stress level.
Stress increases the permeability of the lining of the intestines. This will give the gut microbes access into the immune system and the enteric nervous system.
With the above tips, you should have understood how your gut-brain axis works and how to take care of it.
References;
- The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems: NCBI
- Gut–brain axis: Wikipedia, NCBI, NCBI, NCBI, NCBI, NCBI, NCBI, NCBI
- Stress & the gut-brain axis: Regulation by the microbiome: SD
- Anxiety and Depression: SD, NCBI, NCBI, NCBI, NCBI, NCBI, NCBI, NCBI, NCBI, Cell
- The microbiota-gut-brain axis: neurobehavioral correlates, health and sociality: NCBI
- Probiotics and prebiotics: NCBI, FAO, NCBI
- Behavior NCBI, NCBI, NCBI
- Diet: NCBI, NCBI
- Digestive disorders: NCBI, NCBI, NCBI, NCBI, NCBI, NCBI, NCBI, NCBI