For examination or treatment, amniocentesis is a procedure in which amniotic fluid is removed from the uterus. The fluid that covers and protects a baby during pregnancy is amniotic fluid. Fetal cells and different proteins are found in this fluid.
While amniocentesis can provide useful information about your baby’s health, knowing the risks of amniocentesis and being prepared for the results is crucial.
Why it’s done?
Amniocentesis can be done for various reasons:
- Genetic testing: For such disorders, such as Down syndrome, hereditary amniocentesis requires taking a sample of amniotic fluid and analyzing it.
- Fetal lung testing: Checking for fetal lung maturity means taking a sample of amniotic fluid and testing it to decide whether a baby’s lungs are mature enough for birth.
- Diagnosis of fetal infection: Amniocentesis is occasionally used to test a baby for infection or other diseases. The test may also be performed to determine the magnitude of anemia in babies with Rh sensitization, an unusual condition in which the immune system of a mother creates antibodies on the surface of the baby’s blood cells against a particular protein.
- Treatment: Amniocentesis can be performed to remove excess amniotic fluid from your uterus if you collect too much amniotic fluid during pregnancy (polyhydramnios).
- Paternity testing: DNA from the fetus can be obtained by amniocentesis and can then be matched with DNA from the potential parent.
Genetic amniocentesis
Genetic amniocentesis may provide details about the genetic makeup of your infant. In general, genetic amniocentesis is given when the test findings may have a big effect on fertility management or the ability to continue the pregnancy.
Between weeks 15 and 20 of pregnancy, genetic amniocentesis is normally performed. A higher rate of complications has been associated with amniocentesis performed before week 15 of pregnancy.
Genetic amniocentesis may be considered if:
- You had positive results from a prenatal screening test. Suppose the results of a screening test are positive or worrisome. In that case, you can opt for amniocentesis to confirm or rule out a diagnosis, such as the first-trimester screen or prenatal cell-free DNA screening.
- You experienced a chromosomal condition or a neural tube problem in a previous pregnancy: Your health care provider might recommend an amniocentesis to confirm or rule out these disorders if a previous pregnancy was affected by conditions such as Down syndrome or a neural tube defect, a severe condition affecting an infant’s brain or spinal cord.
- You’re 35 or older: There is a higher risk of chromosomal abnormalities, such as Down syndrome, for babies born to women 35 and older. To rule out these conditions, your health care provider may recommend an amniocentesis.
- You or your partner has a family history of a specific genetic condition or are a known carrier of a genetic condition: Amniocentesis can be used to diagnose a lot of genetic disorders, such as cystic fibrosis, in addition to recognizing Down syndrome and spina bifida, a neural tube defect.
- You have abnormal ultrasound findings: Your health care provider may prescribe amniocentesis to diagnose or rule out genetic conditions associated with irregular ultrasound results.
Fetal lung maturity amniocentesis
Amniocentesis of fetal lung maturity will decide if the lungs of a baby are ready for birth. This form of amniocentesis is performed only if, in a non-emergency situation, early delivery is considered to avoid pregnancy complications for the mother, either by induction or C-section.
Between 32 and 39 weeks of pregnancy, it is normally completed. The lungs of a baby are unlikely to be fully formed prior to 32 weeks.
Amniocentesis is, however, not suitable for everyone. If you have an infection, such as hepatitis B, hepatitis C or HIV/AIDS, your health care provider might discourage amniocentesis. During amniocentesis, these infections may be passed to your infant.
Diagnosing spinal muscular atrophy
A group of hereditary disorders that affect nerve cells in the spinal cord, Spinal Muscular Atrophy (SMA), can be diagnosed in a variety of ways. All of your medical records, where you live, and the age at which symptoms begin will affect how and when you are diagnosed with SMA.
Parents pass on spinal muscular atrophy by defective genes to infants. Your doctor may recommend taking a sample of the child’s DNA during pregnancy if you know that your unborn child is at risk for SMA due to your family medical history (prenatal genetic testing).
This is most commonly achieved by gathering a sample of the fluid surrounding the infant (amniocentesis). It can often include gathering some of the structures that make up the sac that surrounds the baby (chorionic villi).
It is possible to obtain both types of samples by a small, hollow needle inserted into your uterus through your abdomen. But samples of chorionic villi are often obtained through a small, hollow tube (catheter) inserted into your uterus through your vagina.
Between 15 to 20 weeks of pregnancy, amniocentesis is normally performed. Samples of chorionic villi can be obtained as early as ten weeks. The DNA sample will be checked for an abnormal or incomplete survival motor neuron 1 (SMN1) gene after it has been processed, which plays a role in most spinal muscular atrophy.
Risks
Amniocentesis carries various risks, including:
- Leaking amniotic fluid: In rare cases, following amniocentesis, amniotic fluid spills into the vagina. However, the amount of fluid loss is minimal in most cases and stops after one week, and the pregnancy is likely to proceed normally.
- Miscarriage: Amniocentesis in the second trimester brings a minor risk of miscarriage, between 0.1 to 0.3 percent. Research shows that for amniocentesis performed before 15 weeks of pregnancy, the risk of pregnancy loss is greater.
- Needle injury: The baby might move an arm or leg into the path of the needle during amniocentesis. However, severe needle injuries are rare.
- Rh sensitization: In rare cases, amniocentesis may cause the blood cells of the baby to invade the bloodstream of the mother. You will be given an injection of a blood substance called Rh immune globulin after amniocentesis if you have Rh-negative blood and you have not formed antibodies to Rh-positive blood. This will stop your body from developing Rh antibodies that can cross the placenta and damage the red blood cells of your infant.
- Infection: Very rarely, amniocentesis might trigger a uterine infection.
- Infection transmission: The virus can be passed to your baby during amniocentesis if you have an infection, such as hepatitis C, toxoplasmosis, or HIV/AIDS. Know, genetic amniocentesis is normally given when the test findings could have a direct effect on pregnancy management. The decision to have genetic amniocentesis, in the end, is up to you. You can be helped by your health care provider or genetic counselor to consider all the variables in the decision.
How you prepare?
It may be good to have your bladder full during the operation to protect the uterus if you have an amniocentesis performed before week 20 of pregnancy. Until your appointment, drink plenty of fluids.
Your bladder should be empty during amniocentesis after 20 weeks of pregnancy to reduce the risk of a puncture.
Before the treatment starts, the health care provider will clarify the procedure and ask you to sign a consent form. Consider asking someone to accompany you to the social support appointment or to drive you home afterward.
What you can expect?
Usually, amniocentesis is performed in an obstetric outpatient hospital.
During the procedure
Next, the ultrasound will be used by your health care provider to assess the precise position of the baby in your uterus. On an exam table, you can lie on your back and reveal your abdomen. In order to display your baby’s location on a monitor, your health care provider can apply a gel to your abdomen and then use a small device known as an ultrasound transducer.
Next, using an antiseptic, the health care professional can disinfect your abdomen. Anesthetics are not commonly used. During the operation, most women experience only moderate pain.
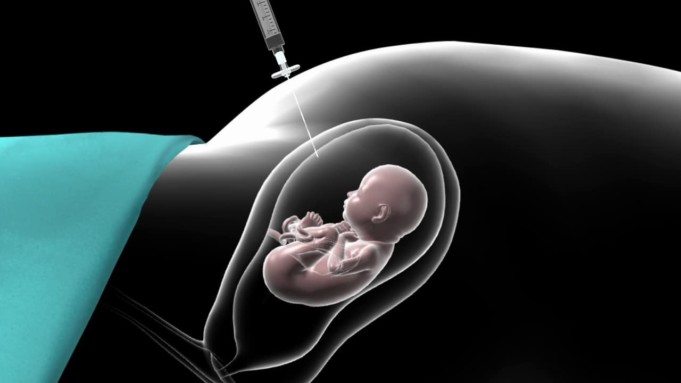
Your health care provider will, directed by ultrasound, insert a small, hollow needle through the abdominal wall and into the uterus. A small amount of amniotic fluid will be removed in a syringe, and the needle will be removed. The exact amount of amniotic fluid removed depends on the progression of the number of weeks of pregnancy.
While the needle is inserted and the amniotic fluid is removed, you may need to lie still. When the needle reaches your skin, you might experience a stinging feeling, and when the needle enters your uterus, you might feel cramping.
After the procedure
Your health care provider will continue to use ultrasound after amniocentesis to control the heart rate of your infant. After amniocentesis, you may experience cramping or slight pelvic discomfort.
After the treatment, you will resume your normal activity level. However, for a day or two, you might recommend avoiding strenuous exercise and sexual activity. In the meantime, the amniotic fluid sample will be analyzed in a lab. Within a few days, some outcomes may be available. Other outcomes may take up to four weeks.
Contact your health care provider if you have:
- Loss of amniotic fluid or vaginal bleeding through the vagina
- Extreme cramping of the uterus that lasts more than a few hours
- Fever
- Redness and inflammation where the needle was inserted
- Unusual fetal activity or a lack of fetal movement
Results
Your health care provider or a genetic counselor will assist you in interpreting the effects of your amniocentesis. Test results for genetic amniocentesis will accurately rule out or diagnose different genetic disorders, such as Down syndrome. Both hereditary disorders and birth defects can’t be detected by amniocentesis, however.
If amniocentesis suggests that your baby has a non-treatable chromosomal or genetic disorder, you can face wrenching decisions, such as whether to continue the pregnancy. Your health care team and your loved ones are finding help.
For amniocentesis of fetal lung maturity, test results will accurately indicate the lung maturity of an infant. This knowledge will provide reassurance that your baby is ready for birth if you need to deliver the baby early.
References:
- Amniocentesis: Mayo Clinic, Healthline