Minimal change disease (MCD) is a type of kidney disease. The kidney is the primary organ for excretory and osmoregulatory in mammals.
It has the functions of removing metabolic waste products, regulating the water content of body fluids, regulating the pH of body fluids; the kidneys also regulate the chemical composition of the body fluids by removing substances that are more than immediate requirements.
The kidney has a rich blood supply and regulates the blood composition at a steady state. The functions of the kidneys, therefore, contribute to homeostasis, ensures that the tissue fluid composition is maintained at an optimum level for the cells bathed by it, and enable the cells to function efficiently at all times.
Minimal change disease is a type of kidney disease characterized by too much protein is lost in the urine. Minimal change disease is one of the leading etiologies of Nephrotic Syndrome in children globally and can also be detected in adults.
Nephrotic syndrome is a non-inflammatory disease of the kidneys characterized by blood protein leaking into the urine, swelling or edema, and degenerative lesions.
Minimal change disease is known over the ages by so many other names in the medical literature, such as:
- Minimal change nephrosis
- Minimal change nephropathy
- Minimal change nephrotic syndrome
- Minimal change glomerulopathy
- Foot process disease
- Nil disease
- Lipoid nephrosis
- Nil lesions
As earlier mentions, the kidneys filter the blood, discarding the natural waste products from the whole body into the urine and returning the vital elements such as proteins and red blood cells back into the bloodstream.
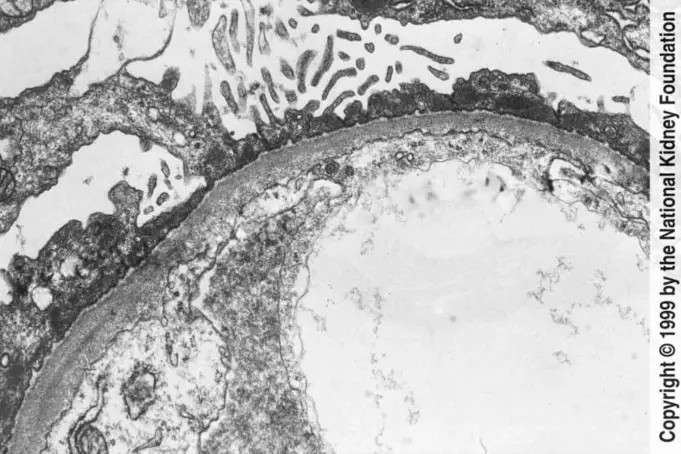
The glomeruli (the ‘sieve’ in the kidneys) are damaged in minimal change disease; however, protein sometimes can “slip through” the filters and escape into the urine. The presence of excess protein in the urine is called proteinuria.
Minimal change disease represents about 15% of patients who are adults with idiopathic nephrotic syndrome. In the younger generation (mostly between 1 to 5 years of age), Minimal change disease is the most common cause of the nephrotic syndrome, accounting for 70% – 90% of patients.
During a puberty period of children, this proportion decreases significantly, unlike other glomerular disorders, such as membranous nephropathy, which becomes more frequent.
Among children, boys seem to be more at risk than girls, about a ratio of 2:1. The prevalence of minimal change disease is seen in about 16 in 100,000 children, be more familiar to South Asians and Native Americas, but scarcer in African American races.
Causes
In mostly adults, Minimal change disease mainly arises as a secondary condition; that is, it is caused by another disease or effect of a drug.
While in children, Minimal change disease is always a primary idiopathic condition; the exact cause is not known, so researchers are actively trying to learn more.
An adult case of Minimal change disease may occur or be in relation to the following:
- Tumors
- Infections caused by a virus.
- Allergic reactions
- Use of certain painkillers called non-steroidal anti-inflammatory drugs (NSAIDs)
Symptoms of Minimal Change Disease
Some of the symptoms of Minimal change disease include:
- Swellings in some parts of the body, such as the ankles and around the eyes. Due to built-up fluid in the body called edema.
- Foamy urine due to large amounts of protein leaking into the urine, a situation called proteinuria.
- Weight gains due to the fluid the body is not able to discard.
- Fatigue
- Loss of appetite
- Nephrotic Syndrome: A group of symptoms that happen together and affect your kidneys. These symptoms include edema, proteinuria, blood protein loss, high levels of fat or lipids in the blood (high cholesterol).
- High blood pressure in some cases
- Low blood Albumin levels
Diagnosis of Minimal Change Disease
The first hints are the signs and symptoms. A doctor may organize tests to help understand the cause of a patient’s symptoms and find the proper treatment for him/her.
These tests include:
- Urinalysis: This is a urine test that helps reveal protein and blood in the urine.
- Blood Test: A blood test will find levels of cholesterol, protein, and supposed waste chemicals in the blood.
- Kidney biopsy: This is a biopsy test where a tiny piece of the kidney is removed with a special collector needle and observed under a microscope. Suppose a kidney biopsy reveals little or no damage under a regular microscope. Minimal change disease diagnosis may be made by presenting other symptoms, such as protein in the urine.
- Glomerular Filtration Rate (GFR): A blood test is done to know how well the kidneys are filtering the body’s wastes.
Because Minimal change disease is always causing nephrotic syndrome in children, they first get treated for Minimal change disease before getting a biopsy. Most persons will have a response in less than eight weeks.
If the protein in the urine disappears, the clinicians may call the disease steroid-sensitive nephrotic syndrome instead of Minimal change disease.
If treatment approaches do not improve symptoms over several months, a biopsy is done to see another cause for the symptoms exist.
Clinical features
- A clinical disorder known as Anasarca may develop. It results in the formation of ascites and pleural and pericardial effusion, leading to abdominal pain because of hypoperfusion or thrombosis.
- Dyspnea is rarely recorded.
- Cold extremities (fingers and toes) associated with low Blood pressure.
- Especially in children, severe infections such as sepsis, pneumonia, and peritonitis may occur during disease onset or later on the course of the disease due to immunoglobin depletion and altered T cell function.
- Frequently, Minimal change disease in childhood-onset in children is preceded by upper respiratory tract infection.
- Intravascular volume depletion and Oliguria (low urine output) are also present.
- Adjoining factors of sepsis, diarrhea, and diuretics can lead to AKI (Acute Kidney Infection, also referred to as Acute Renal Failure), commonly seen in adults.
- Rarely in cases can AKI with gross hematuria followed by anuria secondary to bilateral renal thrombosis.
- The presence of hyperlipidemia is a consequence of increased hepatic synthesis of cholesterol, triglycerides, and lipoproteins.
- Gross hematuria is also rare, occurring in 3% of patients.
- Hematologic parameters may reveal increased hemoconcentrations, which result in increased hemoglobin and hematocrit levels, and thrombocytosis is frequently observed.
Clinically during a diagnosis, there is a reduction in serum total protein and serum albumin (less than 2g/dl), with an increased α2–globulin and a reduced γ-globulin fraction. The decrease in serum protein further reduces total serum calcium, with ionized calcium usually within the normal range. Immunoglobulin A (IgA) is decreased slightly, Immunoglobulin G (IgG) is markedly reduced, while immunoglobulin E (IgE) may be normal or increased, and Immunoglobulin M (IgM) increases.
Treatment of Minimal Change Disease
Minimal change disease is easier to treat than most other glomerular diseases. The first line of medications for treatment in both children and adults with Minimal change disease is corticosteroids such as prednisolone to control proteinuria.
It is necessary to engage a patient in the complete treatment plan of steroids to avoid relapse, as seen in about 70% of cases of Minimal change disease.
For patients who cannot tolerate the corticosteroids, alternatives medications such as cyclosporine, chlorambucil, and rituximab can be used.
Alongside steroidal therapy, diuretics and acute symptomatic management of salt and fluid restrictions to help control edema are recommended by nephrologists.
A medication that blocks a hormone system (rennin angiotensin system) called the ACE inhibitor or ARB is administered to control the blood pressure and low urine protein.
Anticoagulants to prevent blood clots, statins to control cholesterol, and maintaining a correct amount of protein and fluid in diets are some other specialists’ recommendations.
Exercising, not smoking, and vitamin intakes are also beneficial.
Complication
Most patients of Minimal change disease have favorable outcomes without complications. However, a few of these patients experience focal segmental glomerulosclerosis, suffer from severe and prolonged proteinuria.
The complications arising from a Minimal change disease condition are classified into two: Disease-related complications and drug-related complications.
Disease-associated complications include:
- Infections, such as chicken pox, sepsis, cellulitis and peritonitis.
- Thromboembolism, such as venous thromboembolism and pulmonary embolism
- Hypovolemic Crisis such as abdominal pain, tachycardia, and hypotension
- Cardiovascular problems such as hyperlipidemia
- Acute Renal Failure
- Edema
- Anemia
Disease-related complications pathomechanically originate from large loss of plasma proteins especially in the urine of nephritic children.
Other conditions such as hypothyroidism, hypocalcemia, bone disease, and intussusceptions can also arise. The second category of complications arises due to the adverse effects of long-term drug therapy.
Adverse effects of the use of Corticosteroid may include:
- Adrenal Suppression
- Impairment of statural growth
- Peptic ulceration
- Osteoporosis
- Hypertension
- Cataract
- Behavioral changes
- Increased intracranial pressure.
In the use of Cyclophosphamide, adverse effects or complications include:
- Bone marrow suppression
- Alopecia
- Gastrointestinal upset
- Hemorrhagic Cystitis
- Late complications of possible malignancies and fertility impairment.
Long-term use of Cyclosporin A (CsA) which is an immunosuppressive fungal metabolite may cause reduced renal failure, other effects include:
- Hyperkalemia
- Gingival hyperplasia
- Hirsutism
- Encephalopathy
Other medications and possible adverse effects that can result from their usage are:
- Rituximab: Myocardial infarction, progressive multifocal leukoencephalopathy and possibility of reactivation of viruses such as hepatitis B.
- Tacrolimus: Is a calcineurin inhibitor that has similar action to CsA but can have several side effects, such as muscle cramps, tremor, hypertension, renal dysfunction, leukopenia, hyperglycemia, and hypophosphatemia.
- Mycophenolate Mofetil (MMF): Complications from MMF use include gastrointestinal disturbances, bone marrow suppression, and headache.
Summary
Most patients of Minimal change disease are very concerned about Kidney failure as one of the complications of the disease. Well kidney failure is rare for patients with MCD; almost all children and adult patient recover from the condition and long-term relapses are adequately avoided. The major relapse experienced is the presence of protein in urine; this too can be taken care of.
Sources
- Causes of Minimal Change Disease; https://www.medlineplus.gov/ency/article/000496.htm
- Symptoms of minimal change disease; https://www.msdmanuals.com/professional/genitourinary-disorders/glomerular-disorders/minimal-change-disease
- Nephrotic Syndrome; https://www.mayoclinic.org/diseases-conditions/nephrotic-syndrome/symptoms-causes/syc-20375608
- Minimal Change Disease; https://cjasn.asnjournals.org/content/12/2/332