The urinary system, also called the renal system or urinary tract, comprises of the kidneys, ureters, bladder, and the urethra.
The primary responsibility of the urinary system is to eradicate waste from the body, regulate blood volume and blood pressure as well as to control levels of electrolytes and metabolites, and regulate blood pH.
This system can be described as the body’s drainage system for the eventual disposal of urine. The kidneys have an extensive blood supply through the renal arteries, which leave the kidneys through the renal vein.
Each kidney includes functional units called nephrons. Ensuing filtration of blood and further processing, wastes (in the form of urine) leave the organ through the ureters, tubes made of muscle fibres that prod urine towards the urinary bladder, where it is reserved and after that expelled from the body by urination.
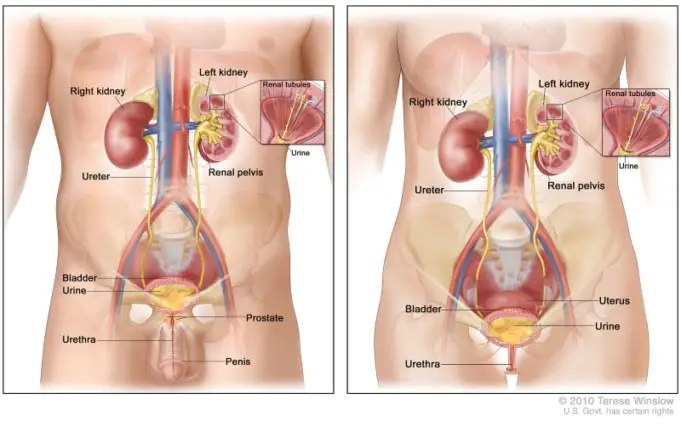
The female and male urinary system are very synonymous, varying only in the length of the urethra. Urine is formed in the kidneys through the filtration of blood.
The urine is then moved via the ureters to the bladder, where it is stored. During urination, the urine is moved through the bladder via the urethra to the outside of the body.
About 0.8 to 2litres of urine is generally produced daily in a healthy human. This amount varies according to the intake of fluid and kidney function
Structure
The urinary system refers to the structures that produce and transport urine to the point of excretion. In the human urinary system, two kidneys are located between the dorsal body wall and parietal peritoneum on both the left and right sides.
The generation of urine begins within the functional unit of the kidney, the nephrons. Urine then flows through the nephrons, through a system of gathering tubules called collecting ducts.
These collecting ducts then merge to form the minor calyces, followed by the major calyces that eventually join the renal pelvis. From this point, urine continues its flow from the renal pelvis into the ureter, carrying urine into the urinary bladder.
The anatomy of the human urinary system varies between males and females at the level of the urinary bladder.
In males, the urethra starts at the internal urethral orifice in the trigone of the bladder, proceeds through the external urethral orifice, and then becomes the prostatic, membranous, bulbar, and penile urethra.
Urine leaves through the external urethral meatus. The female urethra is much shorter, beginning at the bladder neck and ending in the vaginal vestibule.
In many regards, the human excretory or renal system resembles those of other mammalian species, but it has its own distinctive structural and functional peculiarities.
The terms urinary or excretory system underline the elimination function of the system. The kidneys, however, both secrete and vigorously conserve within the body certain substances that are as important for survival
The system contains a pair of kidneys, which regulate the electrolyte constitution of the blood and remove waste products and superfluous quantities of other substances from the blood; the latter substances are urinated, and it passes through the kidneys to the bladder via two thin muscular tubes called the ureters.
The bladder is a sac that retains urine until it is excreted through the urethra.
The urinary system, in humans, as an organ system, contains the kidneys, where urine is created, and the ureters, bladder, and urethra for the passage, storage, and excretion of urine.
Kidney and Nephrons
The kidneys are a pair of bean-like, brown, reddish organs, concave on one long side and convex on the opposite, the Nephrons are found in the kidney. Kidneys and Nephrons are the most complicated part of the urinary system.
Nephrons are the functional part inside the parenchyma of the kidneys, which filter the blood to remove urea, a waste product formed by the oxidation of proteins, as well as ions like potassium and sodium.
The nephrons are composed of a capsule capillaries (the glomerulus) and a small renal tube. The renal tube of the nephron contains an intricate web of tubules and loops that are selectively absorptive of water and ions.
The hormones involved in body regulation will modify the porous nature of these tubules to alter the amount of water that is retained by the body.
This helps the kidneys exercise a significant role in human osmoregulation by regulating the amount of water reabsorbed from the collecting ducts or capsule capillaries in the nephrons found in the kidney, which is controlled by hormones such as renin, antidiuretic hormone, angiotensin I, angiotensin II and aldosterone.
This tubule extends from the capsule. The capsule and the glomerulus are attached and are formed by epithelial cells with a lumen.
A healthy, fully developed human has about 0.8 to 1.5 million nephrons in each kidney. Blood is filtered through three layers: the endothelial cells of the capillary wall, its basement membrane, and between the foot processes of the podocytes of the lining of the capsule.
The tubule has adjacent peritubular capillaries that run between the descending and ascending parts of the tubule.
As the fluid from the capsule flows down into the tubule, it is filtered by the epithelial cells lining the tubule: Osmoreceptors perceive a decrease in water concentration of blood in the hypothalamus( which is in the brain) which stimulates the pituitary glands to secrete antidiuretic hormone to increase the permeability of the wall of the capsule capillaries and tubules in the nephrons.
Therefore, a large amount of water is reeabsorbed, and substances are exchanged (some by addition others are removed), first with the interstitial fluid outside the tubules, and then into the plasma in the adjacent peritubular capillaries through the endothelial cells lining that capillary.
This process oversees the amount of body fluid as well as levels of many body-substances. At the end of the tubule, the remaining liquid is excreted as urine. And it is composed of toxins, water, and metabolic waste.
The extent of blood volume and blood pressure regulation facilitated by the kidneys is a complex process. Besides ADH secretion, the renin-angiotensin feedback system is critically vital to maintaining blood volume and blood pressure homeostasis and Erythropoietin is discharged in response to hypoxia (low levels of oxygen at tissue level) in the renal circulation which stimulates erythropoiesis (for the production of red blood cells) in the bone marrow
Ureter
Urine passes from the renal tube through tubes called ureters into the bladder.
Bladder
The bladder is elastic and serves as a repository until the urine is allowed to pass through the urethra and out of the body.
Urethra
The female and male renal system are very identical, differing only in the length of the urethra.
Function
The primary functions of the urinary system and its organs are to :
- Oversee blood volume, and composition examples are sodium, potassium, and calcium
- Oversee blood pressure.
- Oversee pH homeostasis of the blood.
- Participates in the production of red blood cells by the kidney.
- Enables to synthesize calcitriol (an active form of Vitamin D).
- Reposit waste product (largely urea and uric acid) before it and other products are discarded from the body
Urine formation
Estimated urine production in adult humans is approximately 1–2 liters per day, depending on weight, activity level, environmental factors, health condition of the individual, and state of hydration.
Producing too much or a little urine requires medical attention. Polyuria is a condition of excessive urine production, which is over two and a half liters of urine while Oliguria is when 400 ML daily is produced, and anuria one is when urine production is about 100 mL per day.
The first phase of urine formation is the filtration of blood in the kidneys. In a healthy individual, the organ collects between 12 to 30% of cardiac output, but it averages about 20% or about 1.25 Litre per minute.
The fundamental structural and functional component of the kidney is the nephron. Its principal function is to control the concentration of water and soluble substances like sodium by filtering the blood, reabsorbing what is needed and excreting the rest as urine.
In the first part of the nephron, the bowman’s capsule filters the blood from the circulatory system into the tubules. Osmotic and Hydrostatic pressure gradients enable filtration through a semipermeable membrane.
The filtrate comprises of water, ions, and small molecules that effortlessly pass through the filtration membrane. However, bigger molecules such as proteins and blood cells are hindered from passing through the filtration membrane.
The amount of filtrate generated every minute is known as the glomerular filtration rate or GFR and amounts to 180liters per day. Over 98% of this filtrate is absorbed back into the body as it passes through the nephrons, and the remaining percentage becomes urine.
The endocrine system controls the urinary system using hormones such as antidiuretic hormone, parathyroid hormone, and aldosterone.
The urinary system regulate concentration and volume under the influence of the endocrine system, circulatory system, and the nervous system,
Aldosterone plays a fundamental role in controlling blood pressure through its impacts on the kidney. It functions as the distal tubules and collecting ducts of the nephron and enhances reabsorption of sodium from the glomerular filtrate. Reabsorption of sodium and water retention, which consequently improves blood pressure and blood volume.
Antidiuretic hormone (ADH), is a neurohypophysial hormone in most mammals. Its two main functions are vasoconstriction and
water retention in the body. Vasopressin oversees the body’s retention of water by increasing water reabsorption in the collecting ducts of the kidney nephron.
Vasopressin also enhances water permeability of the kidney’s collecting duct and distal convoluted tubule by inducing translocation of aquaporin-CD water channels in the kidney nephron collecting duct plasma membrane.
Urination
Urination is the excretion of urine from the urinary bladder via the urethra to outside the body. In healthy humans the process of urination is under voluntary control.
In infants, some elderly individuals, or those who have experienced neurological injury, urination may occur as an involuntary reflex. The desire to empty the bladder is felt as an uncomfortable full feeling.
It is highly associated with the fullness of the bladder. In males, this feeling of the need to urinate can be felt at the root of the penis as well as the bladder, even though the neural action associated with a full bladder originates from the bladder itself, and can be sensed there as well.
In females, the need to urinate is sensed in the lower abdomen region when the bladder is full. When the bladder becomes too full, the sphincter muscles will involuntarily relax, enabling urine to pass from the bladder, and urinating is experienced as a decrease of this discomfort.
The male releases urine through the penis, while the female urinates through the vulva.