Unstable angina, also known as crescendo angina or acute coronary respiratory syndrome, is the chest pain that occurs while the body is at rest or with stress or exertion.
Pain from unstable angina worsens frequency and severity and is caused by the blockage of the arteries supplying blood and oxygen to the heart.
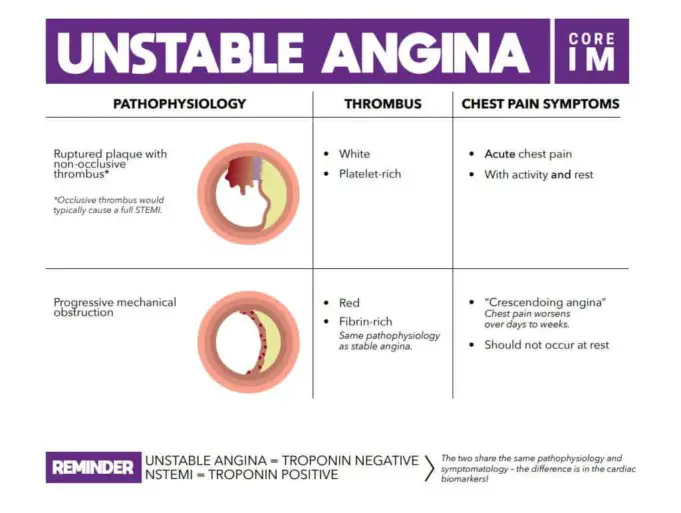
These blockages in the arteries are fatty buildups that rupture, causing injury to the coronary blood vessels, resulting in blood clotting, limiting blood flow.
A case of unstable angina should be treated as a medical emergency. Unstable angina could lead to arrhythmias (irregular heart rhythms), heart attack, or heart failure. It may even lead to death.
Causes and Risk Factors of Unstable Angina
Coronary heart disease is the primary cause of unstable angina. This condition is caused by the buildup of plaque along the walls of the arteries, which causes them to become narrow and rigid.
This blockage limits the flow of blood to the muscles of the heart. Chest pain occurs as a result of insufficient blood and oxygen to the heart muscles.
Risk factors for coronary heart disease include:
- Family history of heart disease
- Obesity
- Diabetes
- High blood pressure
- Being make
- Use of tobacco
- Elevated low-density lipoprotein (LDL) cholesterol
- Low high-density lipoprotein (HDL) cholesterol
- Sedentary lifestyle
Men who are 45 and older and women who are 55 and older are more likely to experience unstable angina.
Signs and Symptoms of Unstable Angina
The major symptom of angina is chest pain and discomfort. The severity of the sensations varies from person to person.
Symptoms of angina include:
- Nausea
- Crushing, squeezing, pressure-like or sharp pain in the chest
- Anxiety
- Pain that radiates to the back
- Dizziness
- Shortness of breath
- Sweating
- Fatigue and weakness
Stable angina can progress to unstable angina. It is important to watch out for pain in the chest even when you are at rest. Also, chest pains that last longer than usual or feel different are usually signs of unstable angina.
Medications like nitroglycerin, which enhance blood flow, typically work for stable angina but not unstable angina.
Diagnosis
The doctor would require a physical examination that includes blood pressure tests to confirm a diagnosis. Other tests that can be used to verify unstable angina include:
- Blood tests to check for cardiac biomarkers and creatine kinase that leak from the heart if the muscle is damaged.
- Echocardiogram, a procedure used to produce images of the heart that reveals blood flow problems.
- Electrocardiogram which is used to observe patterns in the heartbeat that may indicate reduced blood flow.
- Computed tomography angiography (CTA)
- Stress tests
- Coronary angiography and heart catheterization.
Treatment
The treatment for unstable angina depends on the severity of the condition. Treatment options include:
Medication
The doctor may recommend blood thinners like heparin, aspirin, or clopidogrel as a first treatment for the condition. Thinner blood can move more freely through the arteries.
Other medications that can be used to reduce symptoms of angina include drugs that reduce:
- Anxiety
- Arrhythmia symptoms
- Blood pressure
- Cholesterol levels
Surgery
Invasive procedures may be required in cases where there is blockage or severe narrowing in an artery. Surgery options include angioplasty, which involves opening up an artery that was previously blocked.
A small tube known as a stent may also be inserted into the heart to keep the artery.
A bypass surgery may be required in severe cases. The surgery reroutes blood flow from a blocked artery to help improve the flow of blood to the heart.
Lifestyle Changes
A person with unstable angina may need to change certain behaviors to maintain a healthy life. Lifestyle changes that can improve health include:
- Reducing stress levels
- Eating a healthier diet
- Losing weight if overweight
- Quit smoking
- Exercising more
Sources
- Unstable Angina – Healthline
- Unstable Angina – Wikipedia
- Unstable Angina – Heart.org