Have you ever heard of spirometry? This is simply a type of pulmonary function test that is non-invasive and conducted to provide vital information about how well a person’s lungs are functioning.
To be more specific is spirometry reveals how much air moves through your lungs and how quickly the air moves as you breathe through a tube.
A spirometry test is used to diagnose different respiratory conditions like asthma and also to monitor lung diseases so that a doctor can evaluate how well a treatment is working. There are times when spirometry is done in conjunction with other PFT’s usually this depends on the particular information that a doctor is trying to get.
Purpose of a spirometry test
Spirometry tests measure important aspects of lung function. This test can play a crucial role in the diagnosis and management of many lung problems, and you can also use it to distinguish between diseases and conditions that appear to be similar based on symptoms alone.
Spirometry tests are also used for the evaluation of how some lung diseases progress (That is to check if the condition is getting worse, getting better, or if it is staying the same).
This way a doctor can quickly tell if a particular treatment plan is working correctly or if modifications are needed. Nevertheless, it is rare for spirometry to be used alone for the diagnosis of a lung condition.
Usually, it is combined with other things like a patient’s medical history, imaging tests, and physical examination. Spirometry can be used to diagnose the conditions below:
- Emphysema ( a kind of COPD)
- Chronic obstructive pulmonary disease (COPD)
- Bronchiectasis
- Asthma
- Cystic fibrosis
- Pulmonary fibrosis, including idiopathic pulmonary fibrosis.
A spirometry test can also be done before lung cancer surgery to equip a surgeon with vital information about how well a patient will tolerate an operation from a respiratory perspective and also how well the person may respond to having the entire lung or a portion of the lung removed.
Risks and Contraindications
Spirometry is an entirely safe procedure; however, you may become short of breath or feel dizzy and lightheaded while you are taking deep breaths as the test goes on sometimes you may experience coughing.
People dealing with asthma are at a small risk of having an attack during a Spirometry test. On rare occasions, a person might develop a severe breathing problem for a temporary period after a Spirometry test.
Contraindications
- It’s not recommended that a person goes through a spirometry test if they:
- Have chest pain or have recently had a stroke or heart attack.
- Have been dealing with a collapsed lung (pneumothorax).
- Have had an eye surgery in recent time, because the deep breathing needed for spirometry can increase the pressure inside a person’s eyes.
- Recently had chest or abdominal surgery
- Have an aneurysm (bulging blood vessel) in the abdomen, brain, or chest.
- Have a case of tuberculosis (TB)
- Have a respiratory infection, like the flu or a cold
There are some particular conditions under which an individual may not be able to breathe as deeply as required for a spirometry test, and this can tamper with the accuracy of a spirometry test results such conditions include:
- Stomach Bloating
- Pregnancy
- General muscle weakness
- Extreme fatigue
Before the test
Been well informed of what is involved in a spirometry test and the best way for you to prepare can go a long way to help you get the most accurate results from the procedure.
Timing
A spirometry test does not take so much time. It typically takes between 40 to 45 minutes only however if you have plans to spend significantly more time in the hospital then ask your doctor if it will be necessary so that you can schedule the rest of your activities accordingly.
Location
Usually, a spirometry test is carried out in the office of a pulmonologist ( a doctor who specialises only in lung health), or sometimes in a hospital as an outpatient procedure which means that you can go home immediately it is over.
There are cases where you may be required to stay in the hospital overnight, but this would only be necessary if the test is a part of a more extensive test or a procedure like a lung surgery. The analysis is performed usually by a respiratory therapist or a pulmonary function technician.
You can get a spirometry test equipment for home use; however, it is only recommended for use in specific cases which will be discussed below.
What to Wear
Because you will be required to take intense breaths, you should ensure that you dress free clothing that will make it easy for you to breath normal. For example, you may not need to put on a belt or any kind of clothing that will hug or fit tightly around your waist area.
Food, Drink, and Medications
There are a few things you should keep in mind concerning food, drink, and meds:
Eat lightly and drink some water. If you are overfed or stomach is too full, you may find it hard to take deep-enough breaths.
Avoid drinking any kind of alcohol before the test. You may find it challenging to breathe also if you have alcohol in your body, and this could have a negative impact on your test results.
If you are required to take medications, make sure to discuss with your doctor so that your doctor knows what kind of drugs you are taking. Some particular drugs can interfere with your breathing especially medicines that you have to inhale like bronchodilators.
According to the American Lung Association, if you have a short-acting inhaler that you only have to use as needed, make sure that you do not use it for up to six or eight hours before you have your test.
Cost and Health Insurance
For individuals who have a health insurance taking a spirometry test that has been considered medically necessary should be covered at 80% to 100% it all depends on the terms of your policy and also how much of your deductible you have met there is also a chance that you may be responsible for a coinsurance for co-pay.
If you do not have a health insurance the money you’ll be spending out of your pocket for a spirometry test can be as much as $300 and sometimes as less as $30 depending on the region of your country where you having the test done and other factors that may be involved.
The average amount of spirometry is usually around $57 but have it in mind that the money does not include the charges for a doctors appointment. So you may spend an additional $30 to $100 to get your test done.
Aside from your insurance card to present at check-in, you shouldn’t need to bring anything in particular to a spirometry test. To make sure, ask your doctor.
Apart from your insurance card that you will have to present at your check-in, you should not be required to bring anything else in particular to a clinic for your test.
Other Considerations
Here are a couple of other things that you must do before having a spirometry test so that you can breathe properly and get the most accurate results possible from your analysis:
Make sure to go to bed early so you can get plenty of sleep a night before you go for your test. If you are a smoker, it is vital that you avoid smoking for a minimum of six hours before your test. Smoking may have a negative impact on your result.
Avoid doing any heavy exercise or strenuous activity for at least half an hour before your test. It is imperative that you conserve your energy.
During the Test
So you are probably wondering what you would experience during your spirometry test. Well, here is a step-by-step explanation of what you should expect.
You should, however, keep in mind that there may be differences among individual practitioners in how they carry out the procedure.
So if you want a specific description of what you should expect from a particular doctor, then you should ask him or her before your test.
Pre-Test
Before you arrive at the hospital for your appointment, you have to check-in first. The check-in process may include filling a few forms, making sure that your insurance card is photocopied for your files, and also taking care of your co-copy if you possess one.
When your doctor calls you in for your test, you’ll be required to urinate so that you can empty your bladder. After which you will be escorted to the room or the office where your spirometric test will take place.
The respiratory therapist or technician in charge of your check will have your weights and measurements taken or probably just ask for your weight and height.
Make sure that you are truthful, the results of a spirometry test are usually calculated based on what is healthy for an individual who is of a specific age, weight, height, and gender as you. There are times when ethnicity is also a factor.
You will be required by the doctor or technician to loosen your belt or get rid of any piece of clothing or jewellery that might interfere with your breathing.
Throughout the Test
during your test you will have to sit in a chair and maybe be instructed to just breathe normally for a while, this is to prepare you for the real test the technician will proceed to put a clip on your nose so that it is slightly closed and you would have to breathe through your mouth.
In a majority of cases, a small piece of equipment will then be handed to you that you would hold in your hand. This equipment usually has a sterile mouthpiece that is connected to the speedometer which is a machine that is about the shape and size of a home printer the speedometer machine will register the force of your breathing and then create a printout of the results.
If your doctor’s office does not have a regular spirometer, you may encounter a different type especially if you’re not able to go to a separate room.
This other type of spirometer is usually very portable, and the mouthpiece is connected to a tiny handheld device that is generally around the size of a small camera. Sometimes it may display your results immediately or just send them to another printer or computer.
Your therapist will give you some special instructions on how the equipment should be held and the lip placement around the mouthpiece so as to create an airtight seal to prevent air from escaping.
The moment you have mastered how to hold it and how to have it in your mouth without letting air escape, you’ll be told to take a deep breath in and then blow out the same air with as much pressure as you can.
It is very essential that you use as much effort as possible and that you blow out every single air in your lungs so that your lungs become completely empty. A patient expected to do this a minimum of three times and the technician will be with you all through telling you what to do and what not to do.
The spirometer will create a graph that depicts your results and that the technician can read and interpret on the spot. In some cases, if a person’s breathing patterns show an obstruction, he will be asked to use a short-acting bronchodilator such as albuterol to help open the airways and then repeat the test to see if the medication brings about an improvement.
The spirometer will create a graph according to your breathing activity, and this graph will depict what your result is, and the technician will be able to read, understand, and interpret it on the spot. There are cases where a person’s breathing pattern may show that there is an obstruction.
In such a case the person will be asked to make use of a short-acting bronchodilator like albuterol; this is to help open the person’s Airways. Once the bronchodilator has been used, the patient is to repeat the test so the technician or doctor can see if there is any improvement.
Post-Test
After you’ve had your spirometry test done, you do not have to remain in the hospital or stop your normal activities. You can return to living your life the way you used to, and also if you used to take medications, you could go back to making them even though you had to stop them before the test.
Interpreting Results
Since your test results will be ready instantly, it is likely that your technician or doctor will do a review and discuss the results with you at the office.
To do the evaluation and interpretation, all he has to do is go through the standard procedure of reading through the spirometry test.
The first step of reading through the result is to make sure that the test you have done was valid. This is very vital because there are some things that can go wrong during a spirometry test, and these things can alter the accuracy of your test results.
Below are some of the things that can possibly go wrong during a spirometry test and affect your test results:
- The patient was not able to put in the required effort into breathing into the spirometry machine (usually this may be due to pain or illnesses that get worse with each breath)
- A patient did not fully understand the instructions for the test (possibly as a result of a cognitive or language barrier, and sometimes hearing loss)
- Coughing during the exhale or inhale
- The person was unable to create a tight seal around the spirometer mouthpiece, or maybe their teeth or tongue were not correctly placed in front of the mouthpiece.
- There was some sort of deformation of the speedometer mouthpiece as a result of chewing or biting.
For your spirometry test to be considered accurate, The check must not be affected by any of the issues listed above, and the results should be reproduced immediately after the test. This explains why a technician or doctor will require you to repeat the test at least three times.
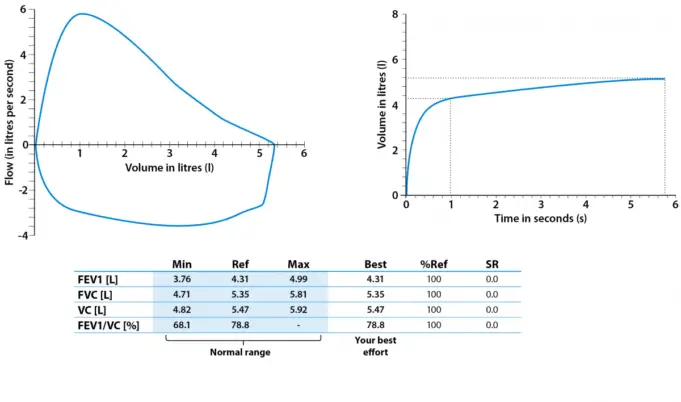
A spirometry provides two crucial measurements of lung function:
- Forced vital capacity (FVC): this is a measure of how much air an individual can blow out of their lungs with a full breath.
- Forced expiratory volume (FEV1): this measures the amount of air an individual is capable of blowing out of their lungs in one second.
To meet the reproducible criteria, all three FVC measurements and all three FEV1 measurements must be within 200ml of each other.
In case any of these conditions are not met, it is concluded that the test has failed to meet the criteria for reproducibility, and the doctor will decide if you must repeat the test and when.
When your doctor is satisfied that the test you did is valid, he or she will then decipher the information that was printed out. The greatest FEV1 and FVC measurements that were achieved represents the patient’s results for the full test.
The doctor or technician will consider these unique numbers and then calculate the ratio of FEV1 to FVC so as to determine if your spirometry is abnormal or normal. An abnormal spirometry results indicate one of three possible breathing patterns:
Obstructive: When a person’s airways are narrowed or obstructed, the amount of air that he or she can blow out fast in one second (FEV1) is usually less than what would be expected on the basis of that person’s weight, age, and height.
To put it differently, an obstructive lung disease causes a person’s lungs to take accept too much air at a time and also take too long to empty. Since in this case, your FEV1 is low, the result will show that the ratio of FEV1/FVC is lower than average.
Something else that will be seen is an obstructive pattern in lung conditions that will affect the airways such as asthma and COPD. The following are the break down of FEV1 values:
- An FEV1 that is greater than 80 per cent of what is predicted is normal
- An FEV1 that is 60 per cent to 79 per cent of what is predicted usually indicates a mild obstruction
- An FEV1 that is 40 per cent to 59 per cent of what is predicted often indicates a moderate obstruction
- An FEV1 that is less than 40 per cent of what is predicted is an indication of a severe obstruction
Restrictive: A restrictive pattern will often be indicated by a low FVC, but will show a standard ratio of FEV1 to FVC (which means that both numbers are decreased proportionately).
A restrictive lung disease is most times linked with chest surgery (often after a lumpectomy for the treatment of breast cancer, or a pneumonectomy, which means the removal of part or all of a lung), scoliosis (curvature of the spine), obesity, sarcoidosis (inflammation of the lungs, lymph nodes, liver, or other tissues), and even scleroderma (this is a buildup of scar tissue in a person’s skin and other parts of their body).
What a restrictive lung problem means is that a person’s lungs contain too little air and does a terrible job of transferring oxygen into the blood in a healthy way.
Combination: It is possible to have a combination of both breathing patterns. This may be seen when an individual has more than one lung disease, e.g. cystic fibrosis and asthma.
If you had to go through the second round of testing after you have used a bronchodilator and you have an improvement in numbers by 12 per cent or more, this confirms that you have asthma.
In the case of a person who has COPD, the outcome of a spirometry test after the use of a bronchodilator can be an indicator of how severe your disease is.
Follow-Up after your test
If your spirometry test alone is not enough to determine with certainty whether you have a restrictive or obstructive lung disease, a combo of two conditions, or even tell what your exact diagnosis is, your technician or doctor may request that you do other pulmonary function tests, like plethysmography that is used to measure total lung capacity.
However, if your technician or doctor is able to come up with a particular diagnosis based on your spirometry test result, then the next step for you will be to discuss treatment—which could include anything from a lung biopsy if there’s the possibility of cancer, to medication for asthma.
Home Spirometry
You can get a home spirometry unit, and it is basically just a simpler version of the kind of spirometry machine that is used in the hospitals. You can use this under some specific conditions with the oversight of a technician or doctor.
Sometimes, our doctor might recommend that you use a home spirometry unit after you have had your in-office test results. With a home spirometry unit, you can regularly monitor trends in your breathing pattern over a specified period so that you can report back to your doctor for example.
With the results of your home’s parametric test, your doctor should be able to fine-tune and modify your treatment pattern better than using only the results from your in-clinic trial.
It is vital that you only use a home spirometry device if recommended by your doctor something else you should know about spirometry devices is that the level of accuracy usually differs according to brand, so your doctor is in the best position to tell you what brand works best.
The use of homes was mystery devices have become common in recent times so you shouldn’t feel weird about having to use one in your home.
We hope that this article has been educating if you have further questions or would like to list suggestions or opinions, please do not hesitate to comment below.