When most of you visit the hospital for a blood group test; among other blood test, after the test is conducted the result is written as follows: O-, AB+, A– or O (neg), AB (pos), A (neg) as the case maybe.
Most of us do not understand the negative or positive signs and we bother not to ask. Well, the sign states the presence or absence of a particular protein (rhesus D antigen) on the surface of the red blood cells, the protein is known as the RHESUS PROTEIN FACTOR.
There are four major types of human blood (blood groups): A, B, AB and O, each of these groups can either be Rhesus factor positive or negative. Your blood group depends on the genes inherited from the parents.
A person being negative or positive depends on how many copies of the Rhesus D antigen you have inherited. An individual can inherit one copy of this antigen from the mother or father, a copy from the both of them each or none at all.
Now been positive or negative does not really affect or cause any damage in the body system or health wise.
What it is?
Rhesus disease can be described as a condition where the antibodies present in a pregnant mother’s blood attacks the blood cells of her unborn baby.
The Rhesus disease is also known as haemolytic disease. Antibodies are parts of the body’s defense (immune) system, they help fight against foreign bodies in the bloodstream.
How does Rhesus Factor Manifest During Pregnancy?
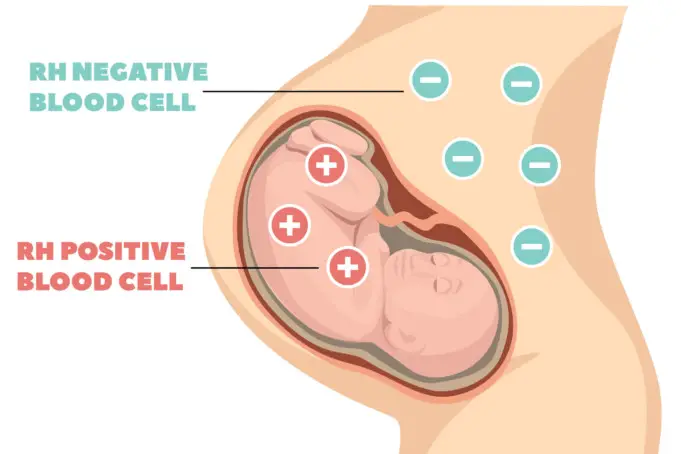
Rhesus factor is very important during pregnancy. If a woman is for instance Rhesus negative (Rh-neg: not having the rhesus factor), and her baby is Rhesus positive (RH-pos: having the Rhesus factor), the woman’s immune system begins to approach the Rh-positive protein in the baby’s blood cells as a foreign body (like an infection) if the immune system is expose to the baby’s blood.
Simply put, if the blood cells from the baby crosses into the mother’s bloodstream, which can occur during pregnancy, labor or delivery, the immune system of the mother will make antibodies against the antigens on the baby’s red blood cells. The Rhesus factor is a rare factor.
If a mother is a Rhesus nagative (RH-neg) blood type, she is categorized as sensitized to positive blood types once her body has made these antibodies; she is placed under surveillance as her body might send these antibodies across the placenta (an organ that connects the baby and the mother) to invade and destroy the baby’s blood cells.
The antibodies can continue attacking the baby’s red blood cells for a few months after birth.
What are the symptoms of Rhesus Disease?
Rhesus disease only affects the baby as the mother is totally safe and will not experience any of the symptoms. The observed symptoms of rhesus disease depend on how severe the condition is in the baby, about 52% of babies diagnosed with rhesus disease display mild symptoms that are easily treatable.
Signs in an unborn baby
- When the baby is still in the womb, a baby that develops rhesus disease might become anaemic as red blood cells are destroyed faster than usual by antibodies.
- If the anaemia persists, signs of complications of rhesus disease such as internal swelling may be revealed by an ultrasound scan.
Signs in newborn
- Heamolytic anaemia: Heamolytic anaemia occurs when red blood cells (the cells responsible for transporting oxygen in the blood) are destroyed. In newborn babies, this may result to pale skins, increased breathing rate due to shortage of oxygen supply, poor feeding and jaundice.
- Jaundice: Jaundice is a condition as a result from a buildup of a chemical called bilirubin in the bloodstream. Bilirubin is a yellow substance that is made biologically from the breaking down of red blood cells. Its level in the blood is normally regulated by the liver; the liver passes out of the body through urine. In infants with rhesus disease, the liver is not able to keep up with the increased level of red blood cell breakdown and high levels of bilirubin when causes the building up of bilirubin in the blood. Yellowing of the skin and eyes are signs of jaundice.
- Lethargy.
- Low muscle tone.
These symptoms might usually not be notable immediately after birth, as it can take up to 3 months after birth before they manifest. Symptoms may subside after completing treatment for a Rhesus incompatibility.
What are the causes of Rhesus Disease?
There are a number of ways that rhesus disease can occur:
- During child labor or delivery
- If the baby is in a breech position and the mother has an external cephalic
- Miscarriage or termination
- Vaginal bleeding
- Some test that may be carried out during pregnancy can be sometimes invasive, such as choronic villus sampling (CVS) or ammiocentesis
- Abdominal trauma and blows to the abdomen
Risk Factors of Rhesus Disease?
Any woman who is Rhesus factor negative and is planning to conceive a child with a man who is Rhesus factor positive or who has an unknown Rhesus factor status is at risk of Rhesus incompatibility.
But, given the very low percentage of individuals with Rh-neg blood type, this does not usually happen.
According to statistics of the Stanford Blood Centre, the percentage is broken down roughly:
| O+ | 37.4% |
| O- | 6.6% |
| A+ | 35.7% |
| A- | 6.3% |
| B+ | 8.5% |
| B- | 1.5% |
| AB+ | 3.4% |
| AB- | 0.6% |
It takes quite a period of time for the body to develop antibodies, so firstborns are not usually affected. However, if a mother becomes sensitized as a result of an abortion or a miscarriage, her first living birth child may be affected by the rhesus disease.
Prevention of Rhesus Disease
Medical advancement has bravely reduced the occurrence of the disease on babies. It is usually prevented by injecting the mother with a medication called ‘anti-D immunoglobin’.
All women during antenatal screening are offered blood tests in order to determine whether their blood is Rhesus factor positive or negative. The medication is offered to rhesus negative women who have rhesus positive partners at 28 and 34 weeks of gestation period.
If concerns of sensitizing events occur, it can be given anytime. The anti-D immunoglobin medication prevents the mother’s immune system from producing antibodies that will attack the baby’s blood; it is very safe for both mothers and babies.
Treatments of Rhesus Disease
In cases of unborn babies developing rhesus disease symptoms, treatments depend totally on the severity of the condition. Intrauterine blood transfusion to the unborn child may be needed in more severe cases.
After successful delivery, the child is admitted into a neonatal unit; a hospital treatment unit that specializes in caring for newborns.
Light treatments after delivery may include:
- Blood transfusion
- Phototherapy for neonatal jaundice in mild cases
- Intravenous immunoglobulin injection
If rhesus disease is left untreated, severe cases can lead to stillbirth. In other case, it can lead to brain damage, deafness and even blindness. However, treatment is usually effective, and these problems are uncommon.
Conclusion
As medical managements advance in the field, it is necessary that patients be followed by high-risk obstetricians/maternal-fetal medicine and talented neonatologists postpartum to ensure the most up to date and appropriate standard care.
Sources
- Symptoms of Rhesus Disease; http://www.nhs.uk/conditions/rhesus-disease/symptoms/
- Rhesus Disease; http://www.stanfordchildrens.org/en/topic/default?id=rh-disease-90-P02498
- Rhesus Disease; http://www.marchofdimes.org/complications/rh-disease.aspx