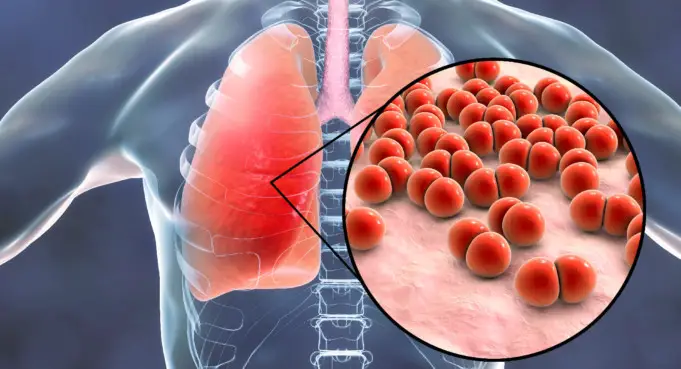
Pneumonia is an infection that affects one or both lungs. It has a wide range of causes with symptoms that can vary from mild to extremely deadly.
It usually starts when the lungs get inflamed by a bacteria, fungi or virus. The alveoli or air sacs in your lungs fill up with fluid or pus, making it difficult for you to breathe in enough oxygen to get to your bloodstream.
Pneumonia can affect anyone of any age. However, people who are at a higher risk of getting affected are children younger than the age of 2 and adult older than 65. This is because their immune system may not be fully developed or too weak to combat the infection.
Is pneumonia contagious?
Pneumonia can be gotten from three sources;
Viruses and bacteria are the leading cause of the illness and are contagious as they can be contacted through inhalation of airborne droplets from a cough or sneeze.
They can also be passed on by coming into contact with objects or surfaces that are contaminated with pneumonia-causing viruses or bacteria.
Fungal pneumonia can be gotten from the environment. But unlike viral and bacterial pneumonia, it doesn’t spread from one person to another.
Are there any risk factors?
Pneumonia can affect anyone; however, certain groups are at a higher risk of getting infected. They include;
- Infants from zero to two years of age
- Adults ages 65 and older
- People with weakened immune systems due to other medical conditions or use of medications like steroids or certain cancer drugs
- Persons who recently recovered from a lung infection like the flu, or a cold.
- Patients who are suffering from specific chronic medical conditions such as cystic fibrosis, heart failure, asthma, diabetes.
- People who are currently or were recently hospitalised, especially if they are or were on a ventilator.
- Persons who take specific type of drugs, smoke or drink alcohol excessively.
- People who have problems swallowing had a stroke, or are suffering from an ailment that causes immobility.
- Individuals who have been exposed to harmful substances like fumes, pollution, and certain chemicals.
What are the types of pneumonia?
Pneumonia can be classified into different types depending on their cause.
- Bacterial pneumonia: countless bacteria can cause this type; however, the most common cause is the bacterium S. Pneumoniae (streptococcus pneumonia).
- Viral pneumonia: this can occur from the flu, also known as influenza, and the respiratory syncytial virus (RSV).
- Fungal pneumonia: this can arise from a condition such as valley fever, resulting from the Coccidioides fungus. This type is not contagious
- Aspiration pneumonia: this can result when liquid food or stomach content is accidentally breathed into the lungs. This type is also not contagious.
- Hospital-acquired pneumonia: this can result in patients being treated for other illnesses — for example, those attached to a breathing machine or respirator.
The signs and symptoms will be similar, regardless of the cause.
Symptoms
Symptoms can range from mild to life-threatening. The first symptoms of the infection resemble those of the flu or cold. The person then develops chills, a high fever, and a cough with sputum.
Common pneumonia symptoms include;
- Headaches
- Nausea or vomiting
- Sweating or chills
- Fever
- Shortness of breath and fast breathing
- Coughing that may produce green or rusty phlegm or sputum
- Loss of appetite or
- Feeling fatigued or tired
- Chest pain that happens when you breathe or cough
Other symptoms can vary according to your general health and age
- Signs may not be visible in infants, but sometimes they may have trouble eating or drinking, or may experience lack energy, vomiting
- Children under the age of five may experience wheezing or fast breathing
- Older adults may experience milder symptoms. They may also experience a lower-than-normal body temperature as well as confusion or changes in mental awareness.
How is pneumonia diagnosed?
Your doctor will begin by requesting for your medical history and then ask you some questions about the symptoms you’re experiencing and when they first appeared.
He’ll then conduct a physical examination on you. This will involve using a stethoscope to listen to your lungs for any abnormal sound like bubbling, crackling or rumbling when you breathe.
Your doctor may also order some more tests, depending on how severe your symptoms are, plus your risk for complications. Such tests include;
Pulse Oximetry
This test is conducted by using a painless monitor known as the pulse oximeter on your finger to measure the levels of oxygen in your blood.
The device can detect whether your lungs are carrying enough oxygen through your bloodstream.
Chest X-ray
Your doctor checks for signs of inflammation in your chest using the x-ray. If swelling is detected, the x-ray can also provide detailed information about the location of the inflammation and how far it has spread.
Blood culture
This test helps confirm an infection using a blood sample. Culturing can also help in identifying the root cause of the condition.
Fluid Sample
Your doctor may carry out this test if he suspects there’s fluid in the pleural space of your chest. It is done by placing a needle between your ribs to extract a fluid sample from your chest. It can help identify what may be causing the condition.
Sputum Analysis
This test is done by taking a mucus sample after you have coughed deeply. The sample is then sent to the lab for proper analysis to pinpoint the cause of the condition.
CT scan
A CT scan provides a clearer and more detailed image of your lungs.
Bronchoscopy
A bronchoscopy directly analyses the Airways in your lungs for blockages or other problems. It is done by passing a bronchoscope (a thin and flexible tube with a camera at one end) through your throat into the lungs. This is done while the patient is on anaesthetics.
Your doctor may resort to this test if you are hospitalised and not responding to antibiotics or if your initial symptoms were severe.
Treatments for pneumonia
Treatments depend on the type of pneumonia you have, its severity and your general health.
Prescription medication
If it’s a case of bacterial pneumonia, you’ll be given oral antibiotics. Make sure to complete the dosage given to you by your doctor, even if you feel better halfway into the medications.
Not completing the dosage may prevent the infection from clearing completely, and it may be difficult to treat in the future.
Antibiotics don’t work for viral pneumonia. It is usually treated with a lot of rest and drinking a lot of fluids.
You doctor may also prescribe an antiviral. However, most cases of viral pneumonia resolve on their own with at-home care.
Fungal pneumonia is treated with anti-fungal medications. It may take several weeks for the medicine to clear the infection.
At-home care
Doctors commonly recommend some over-the-counter medications to help relieve some symptoms like aches and fever, as needed. These may include;
- Acetaminophen (Tylenol)
- Aspirin
- Ibuprofen (Motrin, Advil)
Your doctor may also prescribe cough medicine to manage your cough so you can rest. Note that coughing helps extract fluids from your lungs, so you don’t want to eliminate it completely.
Hospitalisation
You may need to be hospitalised if you experience severe symptoms or you have other health complications. Once there, your healthcare provider will monitor your breathing, temperature, and heart rate. Hospital treatment may include:
Respiratory therapy to maximise your oxygenation by teaching you to perform certain breathing techniques or delivering specific medications directly into your lungs.
Injecting intravenous antibiotics into a vein.
Oxygen therapy to manage oxygen levels in your bloodstream (administered through a face mask, nasal tube or ventilator, depending on the severity of the condition)
Prevention
Many cases of pneumonia can be prevented. Prevention methods include:
Vaccination
This is the first line of defence against pneumonia. There are several vaccines that are effective in preventing pneumonia. They include
Pneumovax 23 and Prevnar 13
These two vaccines are effective against specific types of pneumococcal bacteria responsible for causing pneumonia and meningitis. You, healthcare provider, can tell you which of them is better for you
Pneumovax 23 helps protect against 23 types of pneumococcal bacteria. The Centre for Disease Control and Prevention recommends it for:
- Adults within the age of 19 and 64 who smoke
- Adults aged 65 years and older
- People between the ages of 2 and 64 with chronic illnesses that may increase their risk of pneumonia.
Prevnar 13 helps protect against 13 types of pneumococcal bacteria. The CDC recommends this vaccine for:
- Adults above the age of 64
- Children younger than two years
- People between the ages of 2 and 64 with chronic illnesses that may increase their risk of pneumonia.
Hib vaccine
This vaccine keeps you safe from Haemophilus influenzae type b (Hib), a type of bacteria responsible for causing pneumonia and meningitis. The CDC recommends it for:
- Every child under the age of five years
- Older children who haven’t been vaccinated before or adults with certain medical conditions.
- People who have gotten a bone marrow transplant
Flu vaccine
Be sure to get an annual flu shot as pneumonia may also be a complication of the flu.
The CDC recommends that Vaccination should be given to everyone ages six months and older, especially those who may be prone to flu complications.
The National Institute of Health (NIH) states that pneumonia vaccines won’t protect against all cases of the infection.
However, Vaccination may reduce the symptoms and length of infection as well as lowering the risk of complications.
Other prevention methods
You can also avoid pneumonia by making some routine changes in addition to Vaccination.
- Cover your sneezes and coughs. Properly dispose of used tissues.
- Always wash your hands with soap and water
- If you smoke, try quitting. Smoking makes you more prone to respiratory infections, especially pneumonia.
- Maintain a healthy lifestyle to enhance your immune system. Eat a healthy diet, get enough rest and exercise regularly.