Plantar fasciitis is one of the most common infections that causes pain on the heel of a person’s leg. Generally, in a person’s foot, a thick sheet of tissue(ligament) runs across your foot, i.e., from the bottom of your foot to the heel of the foot.
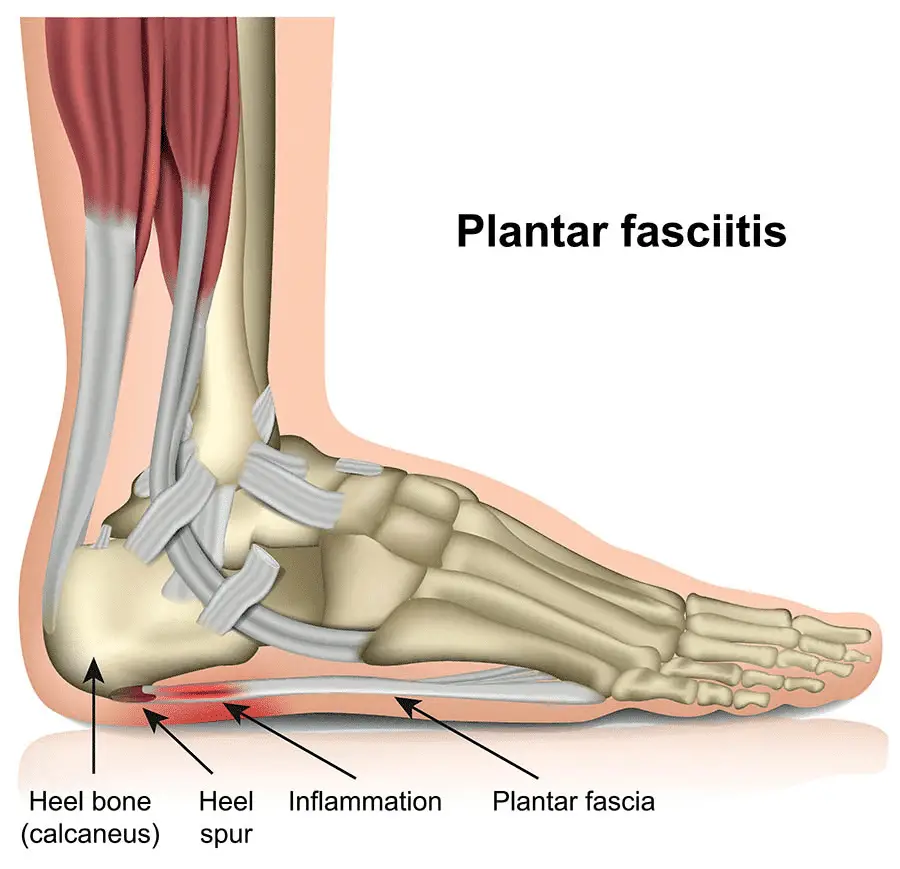
This adhesive sheet of tissue is known as a fascia, and because it is on the foot, it is known as the plantar fascia. When there is an inflammation of this thick sheet of tissue, it results in plantar fasciitis.
Plantar fasciitis is what is responsible for pain in the heel. In everyday life, our ligaments experience a lot of wear and tear, and once the plantar fascia is inflamed, it causes a lot of pain.
Generally, plantar fasciitis is experienced when you take your first steps in the morning. If you get down from your bed and you start to experience severe pains in your foot, but as you move on with the foot, the pains tend to decrease, then you probably are experiencing plantar fasciitis.
This condition is common in runners and most athletes. It is also common in those who are overweight, and even those who wear shoes that don’t help them to balance or probably is too tight on them.
Plantar fasciitis is one of the most common problems that can be seen in orthopedic hospitals these days. Some researchers in a 2003 speculated that this condition might be as a result of a degeneration of the fascia instead of an inflammation. However, most doctors never consented to this.
Causes
The plantar fascia has the peculiar shape of a bowstring. It helps in supporting the arch of your foot when you walk and also helps in absorbing shock. Once the stress and tension on the bowstring become too much, it can result in the tearing of the fascia little by little.
Once the fascia becomes overstretched, and the tearing becomes too much, it will cause the irritation of the fascia, which can lead to possible inflammation.
Although what causes the increase in stress and tension on the fascia remains unclear, some doctors have attributed the causes to heel spurs, although it still hasn’t been proven yet.
Symptoms
The major symptom that one who has plantar fasciitis will experience is severe pains at the bottom of the foot just beside the heel. The kind of pains the patient will experience will feel like a sharp stabbing pain that starts as the person begins to walk.
This pain is usually quite severe when the patient wakes up and tries to stand up. The patient may also experience pain when exercising; however, after exercising, the pain is always increased.
Sometimes, the pain can be felt around the mid-foot. The pain may not start immediately. It can begin as a dull ache and gradually increase over time. The pain may feel like a stabbing pain, or sometimes, it can be as though, it’s a burning ache.
If the patient is experiencing plantar fasciitis, it can result in heel stiffness and, as such, causing difficulties in climbing the stairs. If left untreated, the patient can find it difficult to walk.
Risk factors
Although plantar fasciitis has no known cause, there are certain factors that can increase your chances of developing this condition.
These risk factors include:
1. Age
As you go higher in age, many things in your body begin to decline, and that can result in a lot of problems. Plantar fasciitis mostly occurs in adults who are within the ages of 40-60years of age.
Some adults who are within 60-70 years also may be at risk of developing this condition as well.
2. Sex
According to research, women are much more at risk of developing plantar fasciitis than men. Women who are pregnant may often experience plantar fasciitis. This condition is usually common during the third trimester of pregnancy.
3. Extra weight
If you are overweight or obese, you are at a higher risk of developing plantar fasciitis. This is because your extra weight is putting on additional stress on your lower body, especially your feet.
If you suddenly start gaining weight, you will begin to put additional pressure on your plantar fascia, causing it to stretch. Once it becomes overstretched, tiny tears start occurring in the fascia and, as a result, causing inflammation to occur.
4. Exercises
Some certain kinds of exercises can cause you to keep straining your plantar fascia. Some dances such as aerobic dances as well as gymnastics can result in a lot of stress on your heel as well as the tissues attached, which includes your plantar fascia.
Being a gymnast or a ballet dancer has its benefits, but over time, it can lead to one common problem that these two athletic may people face, which is plantar fasciitis.
5. Foot mechanics or mode of walking
According to doctors, one common reason why women often experience plantar fasciitis more than men is because women usually wear high-heeled shoes.
Although wearing heels is beautiful and makes you have a fashion statement, however, if you wear the ones that your foot isn’t comfortable with or the ones that can result in severe pains because of the amount of inches, then you may be signing up for plantar fasciitis.
People who have flat feet, a high arch, or sometimes an abnormal pattern of walking can result in unequal weight distribution when they are standing and, as a result causing plantar fasciitis.
6. Certain Jobs
If you have a job that keeps you on your feet almost all the time, especially on tough surfaces, it can cause you to develop plantar fasciitis. Factory workers, teachers, engineers, miners, and so on who spend their time at work on their feet are at the risk of developing inflammation of the plantar fascia.
7. Foot problems
People who have certain foot problems such as tight Achilles tendons can cause your plantar fascia to become inflamed, causing plantar fasciitis. Usually, in every human, two muscles come together to form the Achilles tendon.
The tendons of the gastrocnemius and soleus muscles come together to form the Achilles heel. If due to a malformation of the feet, the heel becomes too tight, it will affect the plantar fascia because the fascia is attached to the heel.
However, these heel pains are not the same as heel spurs. Previously, doctors usually believe they were the same thing, although they are similar because of the origin of their pain; however, the causes and symptoms are different.
Diagnosis
Plantar Fasciitis is often diagnosed based on the physical examination conducted on the patient as well as the patient’s medical history. When your doctor is conducting physical tests, he will look out for areas that feel tender in your foot.
Once your doctor can locate the place that feels tender and painful, it can help your doctor diagnose the cause of your pain.
Generally, your doctor won’t require you to go for any tests after the physical examination has been carried out. However, in some cases, your doctor may request that you go for imaging tests.
Your doctor may require you to go for X-Ray or an MRI scan in order to make sure that it is only the plantar fasciitis and not any other underlying problem such a stress fracture that is causing you pain.
Some X-ray scans may be able to detect the presence of a stick of bone shooting out of your heel. Once this is detected, then what you have is a heel spur and not plantar fasciitis. Most people who have heel spurs don’t usually experience pains in their heels.
Treatment options
The majority of people who have plantar fasciitis often recover in a few months after immense conservative treatments. Treatment can include resting, stretching, as well as applying an ice pack on the painful area.
In not so severe cases, your doctor can prescribe the use of medications as well as therapies to help relieve the pain and resolve the issue.
1. Medications
Basically, the medications are to help relieve you of the pain, and as such, your doctor can prescribe certain drugs such as some ibuprofen (such as Advil, Motrin IB), as well as naproxen sodium.
These drugs will help relieve your pain and reduce the inflammation, which is a result of plantar fasciitis.
2. Therapies
As uninteresting and as painful as therapies may sound, therapies are very good when it comes to helping you deal with plantar fasciitis. These therapies will involve stretching and strengthening exercises as well as the use of specialized equipment to help treat the pain.
The kind of therapy your doctor may prescribe include:
i. Physical therapy
This kind of physical therapy is aimed at strengthening your leg muscles, stretching the plantar fascia as well as helping to strengthen your Achilles tendon. Your physical therapist will show you different types of exercises that can help relieve your plantar fascia of the stress.
Your therapist may also help by teaching you how to apply athletic taping, which can help to support the bottom (plantar) part of your foot.
ii. Night splits
If the pains you are experiencing on your heel is too much, your doctor may recommend that you wear splits in the night’s especially while you are asleep. This is to help you stretch your calf and hold the arch of your foot while you are sleeping.
iii. orthopedic supports
Your doctor may recommend orthopedic supports, also known as orthotics, which can help you distribute your body weight evenly.
3. Surgery
If after several months, medications, as well as therapies, don’t help you, your doctor can recommend more invasive methods such as
i. Injections
When the pains become quite severe and unbearable, your doctor may have to inject steroidal based pain relief medications into the part of the leg. However, it is crucial to be very careful with this process and also avoid injecting multiple shots as this can the weakening of the fascia and inevitably causing a rupture.
ii. Shock wave therapy
Extracorporeal shock wave therapy is a procedure in which sound waves are enhanced and directed into the heel of the foot. Doing this will help stimulate the healing of the heel. However, this process is only used for chronic fasciitis.
Although this method is considered to be inconsistent in terms of effectiveness, however, research has shown that this procedure is promising as it has had quite a number of successes.
iii. Ultrasonic tissue repair
This procedure was invented by MayoClinic doctors. This method is a minimally invasive surgery. It involves the use of ultrasound imaging to help guide a probe which is like a needle into the already damaged plantar fascia.
The needle-like probe uses the ultrasound to rapidly cut the damaged fascia away from the part of the fascia that is still functional. Afterward, the damaged tissue is removed through suction.
iv. Surgery
Surgery is often the last resort. Not everyone needs surgery to repair a damaged fascia or to detach it from the heel completely. Surgery becomes an option when other treatments have failed, and the pain is very severe. It can be done using only local anesthesia, and the operation is usually an open surgery.
Home remedies
Without having to go to the doctors, you can carry out some health care tips to help reduce the pain. These tips include:
1. Control your body weight
One of the leading causes of plantar fasciitis is the sudden gain of weight. Hence, if you have plantar fasciitis, it is imperative that you try to control and maintain a healthy body weight. Doing this will help ease the stress on your plantar fascia and, as such, relieving the pains you feel.
2. Wear supportive shoes
When going shopping for footwear, it is imperative that you remember to buy shoes with low heels as well as have thick soles, have extra cushioning, and provide excellent arch support to your feet.
3. Avoid wearing worn-out athletic shoes
It is essential for you to note that once you notice that your shoes are getting worn out, replace them. This is because of you continue using them, they are no longer capable of supporting your heel or cushioning your heel.
4. Change your sport
If your sport or your job is the cause of your developing pains, then you should start thinking of how to get a new job or find a new hobby. It may. It is easy, but it is totally worth it.
5. Don’t forget your ice-pack
If you are feeling severe pains, you can always apply an ice pack to the site of the pain. It will help reduce the inflammation you may be experiencing.
6. Stretches
Simple exercises will help you stretch out your Achilles tendon as well as calf muscles. So don’t forget your stretches.
References;
- Plantar Fasciitis; Mayo Clinic
- Everythung you want to know about plantar fasciitis; Healthline