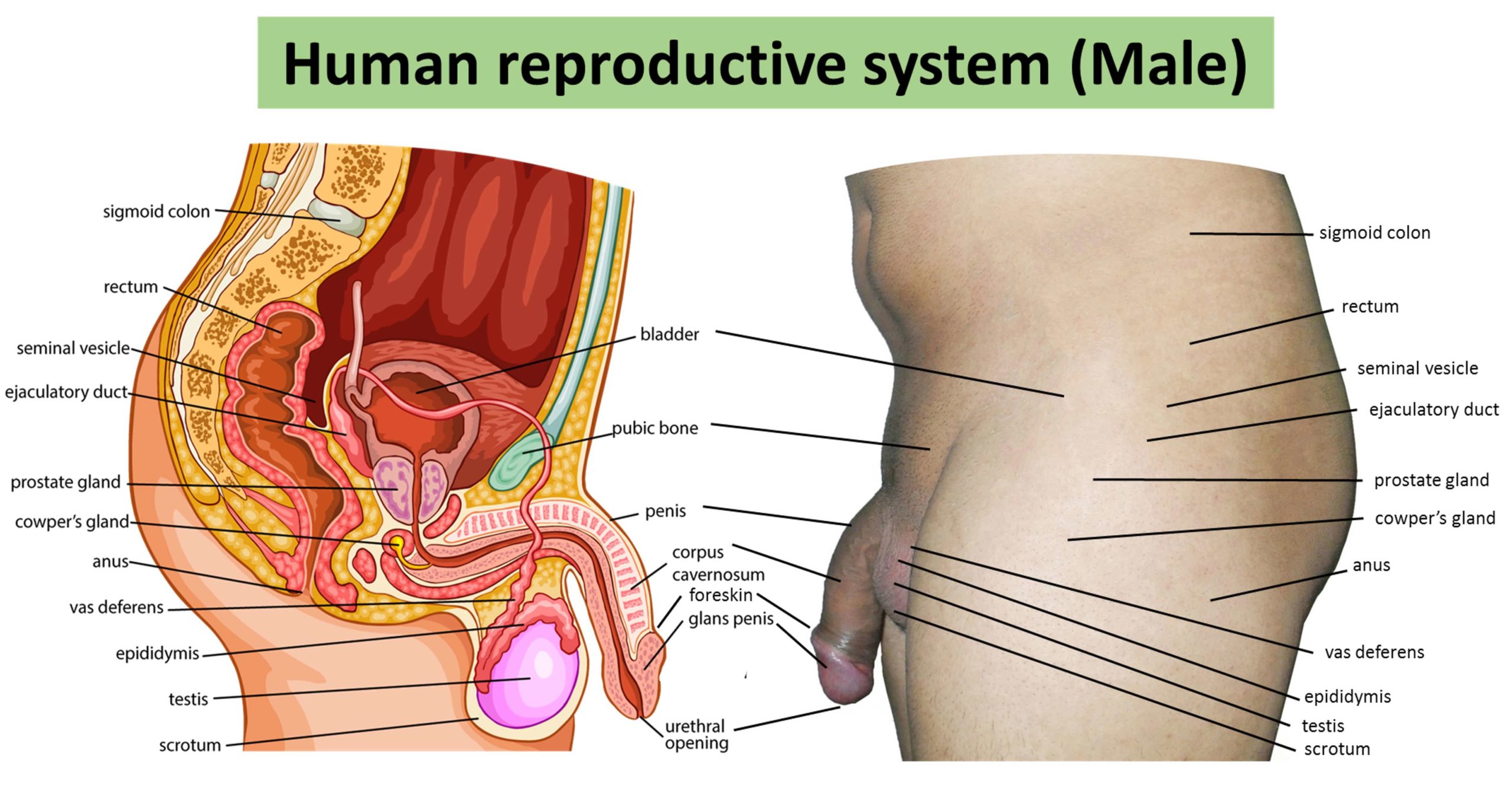
The male reproductive system comprises of several sex organs that aid the human reproduction process. The male reproductive system is a complex network of external and internal organs that operate to support, transport, deliver, and produce viable sperm for reproduction.
Before birth, the male sex organs are created under the influence of testosterone emitted from the fetal testes; by adolescence, the secondary sex organs farther develop and come to be functional.
Sperm is produced in the testes and is conveyed through the ductus deferens, epididymis, urethra, and ejaculatory duct. In the same time, the prostate gland, bulbourethral gland, and seminal vesicles produce seminal fluid that assists and nourish the sperm as it is discharged from the penis during ejaculation.
These organs are located outside of the body and within the pelvis. The main male sex organs are the penis and the testicles, which produce semen, which can fertilize the ovum in the female’s body during sexual intercourse.
The fertilized ovum (zygote) develops into an embryo, which in turn develops into a fetus, which is later delivered as a baby.
Prenatal development of the male reproductive system
The fetal growth of the male reproductive system is the process whereby the reproductive organs develop, establish, and grow during pregnancy.
A zygote is formed with a single fertilized egg and peaks at 38 weeks later with the birth of a male child. It is a part of the phase of sexual differentiation.
The development of the male genital system coincides with the urogenital system. The development of them also can be described together because of the development of the urinary and reproductive organs
Sexual identity of a child is determined at fertilization when the genetic sex of the zygote has been started by a sperm cell containing either an X or Y chromosome.
If this sperm cell embodies an X chromosome, it will co-occur with the X chromosome of the egg cell, and a female child will develop while when a sperm cell carrying a Y chromosome combines an X chromosome, a male child will develop.
The genetic material of the father predominantly determines whether the gonads will be testes or ovaries. In the development of an embryo, after the testes are developed, it will produce and emit male sex hormones during late embryonic development which will result in the production of the male secondary sex organs of the child.
External genital organs of the male reproductive system
Penis
The penis is the external organ that is specially responsible for delivering sperm during coitus. It has an extended shaft, and an enlarged round and bulging tip called the glans penis, which is supported and safeguarded by the foreskin.
The penis becomes erect when ready for sexual activity, which happens because sinuses within the erectile tissue of the penis become engorged with blood.
The arteries of the penis are stimulated and dilated while the veins are restricted so that blood flows into the erectile cartilage under pressure. The pudendal arteries supply the penis blood.
Scrotum
The scrotum is a pouch-like organ that hangs behind the penis. It protects the testicles and also contains several nerves and blood vessels.
The scrotum is an anatomical male reproductive organ that has a double hanging sack of skin and a smooth muscle One testis generally hangs lower than the other to avoid getting squashed in the occurrence of impact.
The perineal raphe is an upright, slightly elevated ridge of the scrotal skin under which scrotal septum is found. It appears as a tiny delicate longitudinal line that runs front to the back of the entire scrotum.
The scrotum contains the testes, epididymis testes, ductus deferens, and external spermatic fascia.
The scrotum is swelling of the perineum and holds some abdominal tissues into its cavity including the testicular vein and artery, and the pampiniform plexus (which forms the principal mass of the spermatic cord, it also functions in venous return from the testes, the pampiniform plexus also plays a vital role in regulating the temperature of the testes. It acts as a cooling device by cooling blood in adjacent arteries to ensure sperm maturation).
The scrotum becomes covered with pubic hair at puberty, and it usually tightens when exposed to cold temperatures and when erect as a result of arousal.
Internal genital organs
Testis or Testicles
This is the male gonad or the male reproductive gland. The testis has two primary functions: to supply sperm by meiotic division of sperm cells within the seminiferous tubules and to synthesize and secrete androgens that regulate the male reproductive processes.
The site of production of androgens in the Leydig cells that are located in the interstitium between seminiferous tubules.
The testes are usually two oval-shaped organs found inside the scrotum and get this shape from some tissues known as lobules. Lobules are formed by some coiled tubes shrouded by dense connective tissues called the “Seminiferous tubules.”
Seminiferous tubules are coiled tubes that make up each of the two testes. The cells and tissues in the tubules aid spermatogenesis, which is the process of sperm creation.
These tubules are covered with a layer of tissue called the epithelium. The epithelium is made up of Sertoli cells that enable the production of hormones that develop sperm.
Among the Sertoli cells are the spermatogenic cells that split and become spermatozoa or sperm cells. The tissues next to the tubules are called Leydig cells. These cells create male hormones, such as testosterone and other androgens.
Rete testis
After sperm is generated in the seminiferous tubules, they travel toward the epididymis via the rete testis.
The rete testis helps to infuse sperm cells into the fluid secreted by Sertoli cells. The body then reabsorbs this fluid as sperm cells travel from the seminiferous tubules to the epididymis.
Before sperm get there, they lack motility, and millions of tiny projections in the rete testis, known as microvilli, help transport the sperm to the efferent tubules.
Efferent ducts
The efferent ducts are a sequence of tubes that enjoin the rete testis to the epididymis. The epididymis stores sperm cells until they’re mature and prepared for ejaculation.
These ducts are lined with hair-like outgrowths called cilia. Along with a layer of smooth muscle, cilia assists the transportation of sperm into the epididymis.
The efferent ducts also absorb most of the fluid that helps to move sperm cells, and this results in a higher volume of sperm in ejaculate fluid.
Three layers of tissue surround the testes. Which are :
- Tunica vasculosa
- Tunica vaginalis
- Tunica albuginea
Tunica vasculosa is the first tiny layer of blood vessels. This layer guards the tubular interior of each testicle from other segments of tissue around the outer part of the testis.
The next layer is named the tunica albuginea. It’s a protective layer made of thick, densely packed fibers that boost the protection of the testes.
The outermost layers of tissue are the tunica vaginalis. The tunica vaginalis contains three layers:
The visceral layer which surrounds the tunica albuginea that insulates the seminiferous tubules.
Cavum vaginalis is a space between the visceral layer and the outermost layer. The parietal layer is the outermost protective layer that encompasses nearly the whole testicular structure.
Epididymis
The epididymis is a long whitish mass of firmly coiled tubes. Sperm produced in the seminiferous tubules usually progress into the epididymis during which the sperm undergo maturation and are concentrated by the action of ion channels located on the apical membrane of the epithelium.
The epididymis consists of three sections and is the head, body, and tail. Although it bears insignificant resemblance to the testes, the epididymis is distinctive in that it is smaller, and the tubes are more substantial and less densely stuffed.
Near the topmost part of the testis is the head of the epididymis, which reserves sperm until it is ready to undergo maturation.
Next is the body, a long twisted tube where the sperm undergoes maturation. This process takes approximately one week. The tail is the last part, and it connects to the deferent duct, also called the ductus deferens or vas deferens.
From this point, the sperm is transferred to the ejaculatory duct. Partially enclosing and separating the epididymis from the testis is a thin sheet of tissue called the tunica vaginalis.
Vas deferens
The ductus deferens also referred to as the sperm duct, maybe a thin tube approximately 30 centimeters (0.98 ft) long that starts from the epididymis to the cavity. It carries the spermatozoa from the epididymis to the duct.
The vas deferens is a little bit larger than of the ductus epididymis (the tube found in the epididymis gland). The tissue lining the inside wall is a furrowed moist layer of mucosal membrane, surrounding this membrane are three layers of longitudinal and circular muscular fibers.
These fibers allow the ducts to contract and which helps the fluids and sperm to be transported. The ductus deferens or vans deferen starts at the tail region of the epididymis, in the lower part of the scrotal sac, the pouch of thin, delicate skin that covers the testes and epididymides.
It stretches into the pelvic region. While edging to the position of the bladder, the ductus deferens is surrounded by a web of nerve fibers, pampiniform plexus veins, and arteries, and layers of connective tissue coat the whole. (This complex tubular structure, called the funiculus, also serves to suspend the testes.).
At the extent of the bladder, each duct separates from its coat of animal tissue and travels back over the crown of the bladder; the two ducts turn below at the rear of the bladder, and their channels widen to form the two ampullae connected to the left and right surface walls of the bladder.
The ampullae act as depository chambers for the semen and contribute secretions to it. The yellow secretions of the ampullae include ergothioneine, a substance that decreases chemical compounds, and fructose, sugar, and nutrient. Both secretions moisten the sperm and help to conserve their viability.
The internal cavities of the ampullae have several meshes like compartments and folds. The walls of the ampulla are narrower than the other parts of the sperm canal, and the channel is usually more significant.
The size of the ampulla varies with different animal species; in man, they are only two times the size of the ductus deferen. The ampullae join the ducts of the seminal vesicles to make up the ejaculatory ducts.
Accessory glands
Three accessory glands provide fluids that lubricate the duct system and nurture the sperm cells. They are the seminal vesicles, the prostate gland, and the bulbourethral glands or Cowper glands.
Diseases of the male reproductive system
The reproductive system is vulnerable to a wide array of diseases and disorders. These are of differing degrees of harm to the body.
This can include testicular torsion, cancer which can develop in reproductive organs such as the testicles and prostate. Diseases of the male reproductive organ are;
- Penile Cancer
- Prostate cancer
- Testosterone deficiency
- Testicular cancer
- Prostatitis
- Male infertility
- Enlarged prostate or Benign Prostate Enlargement BPE
- Erectile dysfunction
- Undescended testicle
- Varicocele or dilated veins around the testicle
- Hydrocele or fluid around the testicle
- Premature ejaculation
- Hypogonadism
- Sexually transmitted diseases such as Chlamydia, gonorrhea, syphilis, etc.