Hyaline membrane disease (HMD) is a respiratory disease that affects newborns, mostly those born prematurely. In this condition, a membrane composed of proteins and dead cells lines the alveoli- microscopic, tiny air sacs in the lungs that take up oxygen breathed in and keep the flow of gas exchange.
When the alveoli are lined by this membrane, it makes the exchange of gas (oxygen and carbon dioxide) difficult and impossible.
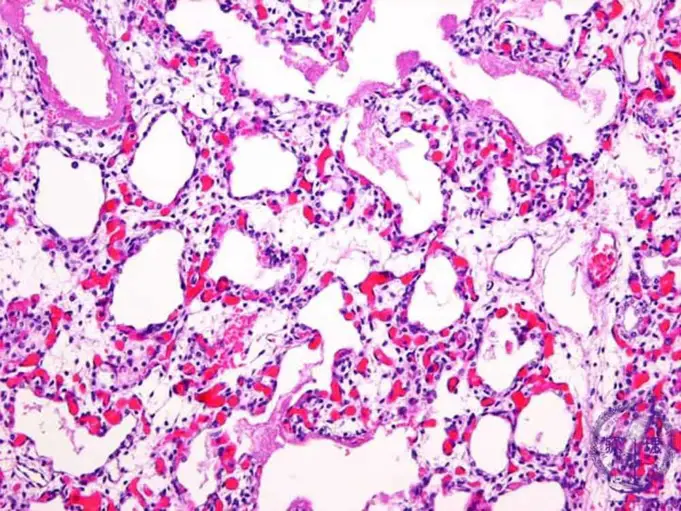
The medical term ‘Hyaline’ originated from the Greek word ‘hyalos’ which means ‘glass or transparent stone (crystal)’. From a microscopic study of the membrane of hyaline membrane disease looks like a glass lining the walls of the alveoli.
In modern times, hyaline membrane disease is referred to as respiratory distress syndrome (RDS); it is one of the most common problems discovered in premature babies and the more premature a baby is, the higher the risk and the more severe the Hyaline membrane disorder.
The disease is traced to a deficiency of a molecule called surfactant. Surfactant is a fluid mixture made of phospholipids and lipoprotein; it is secreted by the cells of the lungs (alveoli).
This fluid serves to reduce the tension of pulmonary fluids and contributes to the elastic properties of the pulmonary tissue, preventing a collapsing of the alveoli during respiration.
The area between the portion occupied by air and the portion occupied by pulmonary fluid is the lining where gaseous exchange occurs. This process of exchange exerts a large force that causes the alveoli to close completely if a surfactant is deficient. Lung compliance is decreased, and the lung becomes stiff and the work of inflating this stiff lung is increased.
As the infant’s lung function decreases due to surfactant deficiency, less oxygen is taken in and more carbon dioxide builds up in the blood. This can lead to acidosis, a condition of increased acid in the body that can affect other body organs.
Hyaline membrane disease condition handicaps a preterm newborn because the ribs become easily deformed; increase in breathing efforts causes a deep sterna (breastbone) retraction resulting in poor air entry.
This results in diffuse atelectasis (collapse of the lungs). Without treatment, HMD typically worsens over the first 48 hours as the baby becomes exhausted trying to breathe and eventually gives up.
But can improve with treatment condition, a mechanical ventilator, also known as a breathing machine, must do the work instead. However, more than 90% of premature babies with HMD survive.
Some factors or conditions can determine the course of Hyaline membrane disease; HMD depends on the size and gestational age of the infant, the severity of the disease, the presence of an infection, whether or not the baby needs mechanical help to breath and if the baby has a patent ductus arteriosus (a heart condition).
Risk Factors of Hyaline Membrane Disease
60 to 80 percent of babies born before 28 weeks (7months) gestation and 15 to 30 percent of those born between 32 and 36 weeks (8 to 9 months) are affected by hyaline membrane disease.
About 25 percent of infants delivered around 30 weeks develop a hyaline membrane condition severe enough to require a mechanical ventilator.
Premature babies are at the highest risk of developing hyaline membrane disease as studied cases reveals that most babies with hyaline membrane condition are premature.
But other factors may increase the chances of a newborn having hyaline membrane disease.
These other risk factors include:
- Cesarean (C-section) delivery
- Caucasian or male babies
- Lack of air immediately before, during or after birth (Perinatal asphyxia)
- Previous birth of baby with HMD
- Perinatal infection (infection immediately before, during or after birth)
- Cold stress (a condition that reduces surfactant production)
- Twin or multiple births (multiple birth babies are often premature)
- Babies with patent ductus arteriosus
- Infants of diabetic mothers; too much insulin in the baby’s system due to maternal diabetes can cause a stress on surfactant production.
Causes of Hyaline Membrane Disease
Hyaline membrane disease typically occurs when there is not enough production of surfactant in the lungs. Surfactant is a fluid produced in the lungs that keeps the airways (alveoli) open.
Surfactant makes it easy for infants to breathe in the air after delivery. Production of surfactant in an infant begins about 26 weeks into pregnancy. Babies born before then or immediately after that period may develop hyaline membrane disease.
Insufficient production of surfactant causes the alveoli to collapse with each breath. As the alveoli collapse, damaged cell accumulates in the airways of the respiratory system and these further hinder breathing.
As hyaline membrane disease progresses, babies have to work harder and harder to breathe trying to re-inflate the collapsed airways.
Symptoms of Hyaline Membrane Disease
Commonly observed symptoms of Hyaline membrane disease immediately after birth include:
- Manifestations of fast breathing (tachypnea: more than 60 breath per minute)
- Increased heart rate
- Cyanosis (blue skin color)
- Chest wall retractions
- Nasal flaring
- Expiratory grunting
As the disease progresses, the baby may develop:
- Ventilator failure (due to raise carbon dioxide concentration in the blood)
- Apnea
Symptoms of hyaline membrane disease usually reach its peak by the third day and may resolve quickly when the baby begins to diuresis (excrete excess water in urine), require less oxygen and a mechanical help to breathe.
These symptoms of HMD may look like other respiratory health disorders.
Diagnosis of Hyaline Membrane Disease
Hyaline membrane disease mostly occurs preterm babies, it is usually diagnosed by the following methods:
- Physical Examination: The first examination for the diagnosis of hyaline membrane disease involves the observation of the baby’s appearance, color, and breathing efforts. These help point to a baby’s need for breathing.
- Chest X-ray: Chest X-rays of the lungs reveals images of the bones and organs. Chest X-rays also demonstrate decreased lung volume (bell-shaped chest), absence of the thymus (after about 6 hours) and a small, discrete, uniform infiltrate that involves all lobes of the lung and air-bronchograms. This infiltrate appears like an outline of the larger airway passages in the case of HMD.
- Blood gas test: This measures the amount of oxygen, carbon dioxide, and acid in the blood. The test may reveal low oxygen and higher amounts of carbon dioxide.
- Echocardiography: This test is a test that functions as an ultrasound, it shows the structure of the heart and how it’s working. The test is mostly conducted in order to rule out heart problems that might cause symptoms similar to hyaline membrane disease. It also shows if a PDA (patent ductus arteriosus) will worsen the condition.
Treatment of Hyaline Membrane Disease
When diagnosis reveals the presence of a hyaline membrane condition in a baby; First of all, oxygen is given with a small amount of continuous positive airway pressure (CPAP), and intravenous fluids are administered to stabilize the blood sugar, salts and blood pressure.
When the condition of the baby is observed to worsen, an endotracheal tube (breathing tube) from a ventilator (breathing machine) is inserted into the baby’s windpipe (trachea) and intermittent breaths are administered by the machine.
Pulmonary surfactant may be prepared either synthetically or extracted from an animal’s lungs, the exogenous fluid is administered into the lungs through the breathing tubes.
This surfactant medication decreases the risk of death for hospitalized low weight babies by 30%. Ventilation may be required for months in very low-weight babies.
Another treatment approach for hyaline membrane disease is extracorporeal membrane oxygenation (ECMO), the treatment entails providing oxygenation through an apparatus that imitates the gas exchange process of the lungs.
However, the downside of this treatment method is that it cannot be placed on babies who are less than 4.5 pounds (2kg) in weight, due to their extremely small blood vessels for cannulation.
These small blood vessels will hinder adequate flow because of limitations to cannula size and subsequent higher resistance to blood flow.
Recently, consecutive successful cases studies have proven a treatment method invented and pioneered by Henrik Verder known as INSURE (intubation-surfactant-extubation) method for managing early hyaline membrane disease.
The method itself has been shown, through meta-analysis, to successfully decrease the use of mechanical ventilation and lower the incidence of Bronchopulmonary dysplasia (BPD).
The method has academically been cited in more than 500 papers since its conception in 1989, which the first randomized study published in 1994 and the second randomized study involving infants less than 30 weeks gestation age in 1999.
The vender worked over the years to improve the outcome of HMD by combining lung-maturity diagnostics with INSURE. The lung-maturity diagnostics included microbubble test, lamella body counts (LBC), and measurements of lecithin-sphingomyelin ratio (L/S) with chemometrics.
Complications
In some cases of hyaline membrane disease, there may result to some medical complications in the course of its treatment. The higher the severity of the disease case, the greater the risk of complications during treatment.
Common occurring complications include:
- Leaking of air from the lung into the chest; when air leaks into the space between the two pleural sacs containing the lungs, is causes peumomediastinum. Also, air leaks may get between the chest wall and the outer tissues of the lungs (pneumothorax), when it leaks into the sac surrounding the heart; it results in a case of pneumopericardium.
A major frequently occurring complication is the pulmonary interstitial emphysema (PIE) that occurs when air leaks is trapped between the alveoli.
- Broncho pulmonary dysplasia (BPD) is a chronic lung disease which causes breathing disorder.
Prevention of Hyaline Membrane Disease
The most effective way to avoid the occurrence of hyaline membrane disease is the prevention of preterm births. But in situations where preterm birth cannot be avoided, administration of corticosteroids to the mother before delivery can dramatically lower the risk and severity of Hyaline Membrane Disease (HMD) in the infant.
These medications are often administered to mothers who are at risk of early delivery, 24 to 34 weeks gestation.
Summary
Hyaline membrane disease (HMD) is a very common medical condition in premature babies. It makes the babies need extra oxygen and assistance with breathing. Hyaline Membrane Disease (HMD) occurs mostly in babies born before the 28th week of gestation but it can also occur in babies before 34 weeks of gestation.
The condition is swiftly progressive and peaks up at day 3, if not treated quickly; the baby will die from suffocation. Treatment involves administering extra oxygen to the baby through breathing tubes from a breathing machine or ventilator.
The disease can as well be prevented by preventing preterm births or administering the mother with corticosteroid medications from 24 weeks of gestation if a preterm birth cannot be avoided.
The corticosteroids stimulate the production of surfactant in the baby’s lungs.
Source;
- Hyaline Membrane Disease; https://www.sciencedirect.com/topics/medicine-and-dentistry/hyaline-membrane-disease
- Hyaline Membrane Disease; https://pediatrics.aappublications.org/content/42/5/758
- Hyaline Membrane Disease; https://radiopaedia.org/cases/hyaline-membrane-disease
- Surfactant Deficiency in Hyaline Membrane Disease; https://www.atsjournals.org/doi/full/10.1164/ajrccm.161.4.16142