When you come across such a name for a disease or condition either while surfing the internet, a book, or hear it from a conversation, the first thought that comes to mind is “weird or strange.”
Hailey-Hailey is just a standard terminology for this disease. It is medically known as familial benign chronic pemphigus; I bet this name will be difficult to remember, so let us stick with the name- Hailey-Hailey in the course of this study.
The Hailey-Hailey disease is a genetic disease; that results from a faulty, abnormal gene. It is a rare inherited skin condition characterized by red scale-like areas that are itchy and creates sores appearing on the skin.
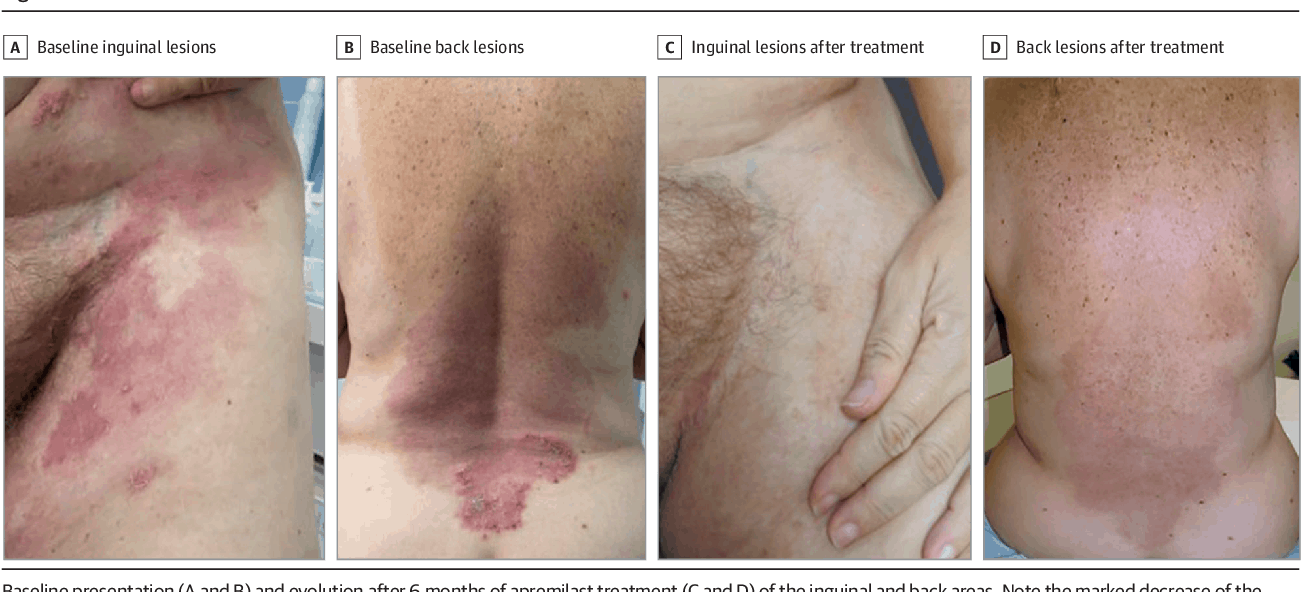
This dermatological condition leads to superficial blisters and broken (eroded) areas of the skin folds, especially in the groin, armpits, neck, and under the breasts.
The Hailey-Hailey disease comes as intermittent flares and tends to appear and disappear to any person. It is a nuisance rather than a serious or emergency problem.
Genetically, Hailey-Hailey disease is defined as an autosomal dominant genodermatosis characterized by intraepidermal vesicles located predominantly in the intertriginous area.
These vesicles may progress to bullae (lesion) then ruptures to form a crust. It is inherited among family members with a 50% chance of inheritance from an affected parent.
In severe cases, persons with Hailey-Hailey disease experience severe pain in affected areas of the skin alongside the development of superficial blisters.
The name Hailey-Hailey was coined by the Hailey brothers (Hugh Edward and William Howard), who first described the condition in 1939.
The Hailey-Hailey condition mostly first appears between age 15 and 40 years, with an average usually occurring during the second and third decades of life.
The severity of Hailey-Hailey disease varies, and it is very unpredictable. Red, itchy, raw, scaly, and superficial blisters areas appear on the skin, usually under the breast, folds of the arms, neck, and groin.
Areas of tight frictions in the body where fresh air rarely gets to are places that may produce much sweat under sunlight and heat. The condition improves with age, and it has no sex preference, as it occurs in females and males, also affects all races.
The Hailey-Hailey disease is a rare disorder that affects 1 in every 50,000 persons. A Hailey-Hailey disease condition may be complicated by secondary infection with scabies, bacteria, herpes, or yeast.
Causes of Hailey-Hailey Disease
The Hailey-Hailey disease occurs due to a mutation in a specific gene that creates a protein essential for the proper development of the skin. Blistering areas in affected persons may be induced and aggravated by trauma, heat, UV light, or perspiration.
Hailey-Hailey disease genetic mutation occurs in the ATP2C1 gene located at chromosome 3. The ATP2C1 gene contains genetic coding for creating a protein hSPCA1.
The protein acts as a calcium and magnesium pump in a cell. This protein pumps calcium ion or magnesium ion into a specialized organelle in the cell known as the Golgi apparatus.
In the cell, calcium has the function of adhering cells to each other, thereby increasing stability and tissue integrity, but when the calcium pump does not function well, the affected tissue will begin to fall apart as its cells will not stick together. This result malfunction damages the skin (a condition known as acantholysis).
The protein hSPCA1 is most active in keratinocytes, the main (primary) type of cells found at the epidermis (outermost layer of the skin). Although the full transition of how improper function of the protein product of ATP2C1 gene causes Hailey-Hailey disease has not yet been fully comprehended.
Still, it is well known that the failure of keratinocytes to stick together results in the blistering symptoms of the disease.
Risk Factors of Hailey-Hailey Disease
According to Malchus et al. 1986, some factors that are known to induce or aggravate Hailey-Hailey disease include:
- Friction
- Heat
- Profuse sweating
- Ultraviolet radiation
- Usually becomes apparent around puberty.
- Infection
- Family history of the condition
- Sunburn or continuous exposure to sunlight
Symptoms of Hailey-Hailey Disease
Symptoms and severity of Hailey-Hailey disease vary between individuals, even among members of the same family. A person may not present all the symptoms clinically mentioned below, but at least two or three are found in every case of Hailey-Hailey disease.
The condition first appears as an erosive, blistering skin rash in regions earlier mentioned in this study. These lesions become itchy and cause a burning sensation, and it may develop into a yellow crusty overlying layer on the skin. The lesions may separate, leaving painful and broken skin.
Secondary infection of the skin lesions may also occur and may cause an unpleasant odor. The skin lesions of a Hailey-Hailey disease case are generally mostly relapsing and remitting; the time of remitting and relapse also varies between persons. When the lesions heal, they do not leave behind scars.
Summarily, from observed cases, the clinical presentations of Hailey-Hailey disease include:
- Burning sensations, often malodorous lesions
- Popular, verrucous, annular, and vesiculopustular variants are rare.
- About 35% of cases are sporadic
- Healing accompanied by hyperpigmentation.
- No scarring
- Longitudinal leukonychia: 70% of patient’s asymptomatic white longitudinal bands on the fingernails.
- Super-infection by Candida albicans, herpes virus, and Staphylococcus aureus
- Cases of complication by squamous cell carcinoma have been reported.
Diagnosis of Hailey-Hailey Disease
Diagnosis is made based on thorough clinical physical examination, a detailed investigation of patient medical and family history, identification of characteristic findings, and also a variety of specialized tests, including biopsy of affected skin tissue.
A Biopsy may reveal keratinization- abnormal formation of keratin tissue (made up of keratinocytes) and failure of cell-to-cell adhesion.
There is no use for blood tests, as antibodies would not be detected, which rules out any differential diagnosis of an autoimmune disorder such as pemphigus.
Molecular genetic testing for mutation in the ATP2C1 gene is also available for confirmation of diagnosis for Hailey-Hailey disease.
Differential diagnosis
A disease must be confirmed through diagnosis, and differential diagnoses of other secondary conditions that may present similar symptoms as the disease of primary focus must be excluded. Comparisons may come in handy during a differential diagnosis.
Some other conditions that may show similar symptoms as Hailey-Hailey disease include:
- Darier’s disease (keratosis follicularis) is another rare genetic skin condition characterized by the development of hard, scaly, progressive rough bumps (papules). The condition is spread with time, like Hailey-Hailey disease, it is a relapsing and remitting condition.
- Intertrigo
- Extramammary Paget Disease
- Tinea Corporis
- Tinea Cruris
Pemphigus is a general term for autoimmune blistering skin conditions. The Hailey-Hailey disease bears it as an alias name due to its resemblance with other pemphigus diseases.
Pemphigus is an autoimmune disorder, that is, a condition that occurs when the body’s immune system attacks the healthy body tissues.
It features a blistering eruption of the epidermis. Types of Pemphigus include:
- Drug-induced Pemphigus
- IgA Pemphigus
- Paraneoplastic Pemphigus
- Pemphigus Erythematosus
- Pemphigus Foliaceus
- Pemphigus Vulgaris
- Pemphigus Herpetiformis
Complications
Some other secondary conditions may arise due to repeated episodes of Hailey-Hailey disease. Most common complications of Hailey-Hailey disease include risks of secondary bacterial, fungal or painful viral infection (eczema herpeticum), which may require antimicrobial agents. Others are Cellulitis, abscess formation, and depression.
For some patients, Hailey-Hailey disease is a mild condition, but for others, the pain and smell can be a severe problem.
Treatment of Hailey-Hailey Disease
The Hailey-Hailey disease has no cure, and treatments are targeted at easing a patient’s symptoms and prevent future recurrence.
Generally, patients are advised by primary health clinicians to:
- Wash and dry skin folds carefully twice daily using mild soap and water.
- Avoid trigger factors like UV light or sunburn, sweating, and friction, tight clothing; when hot, to stay indoors with a fan or air-condition.
- Try to decrease body fat if obese to decrease friction.
- Apply wet compresses, for example, diluted aluminum acetate or vinegar, to dry up oozing patches.
- Apply zinc paste to inflamed patches.
- Take bleach baths twice a week to reduce superficial infections.
- Make use of antiperspirants such as roll-on and cream form of aluminum salts and dusting powders containing the anticholinergic drug diphenyl 2%.
Oral Prescriptions that may be recommended by pharmacists may include:
- A long course of antibiotics such as tetracycline
- If in a case of herpes virus infection, an oral antiviral drug such as acyclovir are prescribed.
- To reduce excessive sweating- hyperhidrosis; anticholinergic medications may be prescribed.
- A few other oral medications like retinoids, ciclosporin, and dapsone have been reported in single cases as partially effective, but they are still in trial stages.
Topical prescriptions or medications that an individual can externally apply to the localized portion of the affected skin part include:
- Corticosteroid creams for short-term application (1-2 weeks) are very effective in treating inflamed lesions.
- Antibiotic ointments such as clindamycin and mupirocin are used for localized infections. It is best used on a short-term basis due to the risk of inducing bacterial resistance when used for the same period.
- Benzoyl peroxide is a very useful antiseptic available as a cream and wash.
- The use of Ketoconazole cream can be employed in case of fungal infection.
- Other effective topical creams used against Hailey-Hailey disease include calcipotriol cream, Fluorouracil cream, and Calcineurin inhibitors (such as Pimecrolimus cream and Tacrolimus cream) have been discovered to reduce the need for topical steroids.
Other treatment approaches against Hailey-Hailey disease are:
- Laser therapy has been reported to be useful. For instance, CO2 laser vaporizes the affected skin, or pulsed dye laser enhances wound healing.
- Phototherapy has also been useful.
- Corticosteroid injections into inflamed plaques
- In more severe cases, surgeries can be performed to remove the affected skin. skin grafts are used to repair the wounds.
- Dermabrasion has been reported to give excellent long-term results.
- Some patients have been reported that have an improvement in Hailey-Hailey disease when treated with low-dose naltrexone.
Summary
A case of Hailey-Hailey disease is not contagious, and it is not an allergic reaction as most misconception suggests. Hailey-Hailey condition is inherited in a pattern known as ‘autosomal dominant inheritance,’ meaning that there a 50% chance that each child of an affected parent would inherit the disease.
The condition is known to improve with age, and several treatment options are available for a patient with Hailey-Hailey disease to choose from.
Sources;
- Hailey-Hailey Disease; http://www.rarediseases.info.nih.gov/diseases/6559/hailey-hailey-disease
- Hailey-Hailey disease: the role of azathioprine an immunomodulatory;
- http://www.panafrican-med-journal.com/content/article/32/65/full/
- Hailey-Hailey Disease (Familial Benign Pemphigus); http://www.medicinenet.com/hailey-hailey_disease_familial_benign_pemphigus/article.htm
- BENIGN CHRONIC PEMPHIGUS; BCPM; http://www.omim.org/entry/169600












