Chromoblastomycosis is a severe fungal infection that is characterized by swollen lessons that can damage the skin, including the subcutaneous tissues. The limbs are generally affected by this condition.
Although chromoblastomycosis is a complication that can affect anyone around the world, it is common in rural parts between 30°N and 30°S latitude with Japan and Madagascar being mostly affected.
More than two-thirds of affected people are male between the ages of 29 and 49. It is also speculated that genetic factors may be involved as well. Other names that the infection is known by include Cladosporiosis, Fonseca’s disease, Pedroso’s disease, Phaeosporotrichosis, or Verrucous dermatitis.
Causes
Chromoblastomycosis may be caused by several fungi found in wood, soil and decaying plant material. The organism is introduced into the skin through an injury, like a cut. The condition is rare in parts of New Zealand, but relatively common in warmer parts such as the Pacific Islands.
These organisms include the following:
- Fonsecaea compacta
- Cladophialophora carrionii
- Phialophora verrucosa
- Fonsecaea pedrosi
- Rhinocladiella aquaspersa (Ramichloridium cerophilum)
Clinical features of chromoblastomycosis

Chromoblastomycosis is generally characterized as a single lesion on an open site such as the hand or foot.
- It starts as a tiny grey or red bump
- It spreads very slowly with about 2mm yearly
- Then it develops into a warty dry nodule or plaque
- Affected persons may notice some partial clearing with scarring in the middle of the lesion
- Affected limbs can develop elephantiasis (enlarged)
- Fresh lesions may appear as satellites around the parent infection
- No discomfort may be felt, but affected persons may suffer itchiness
- Although rare, SCC (squamous cell carcinoma) may develop within longstanding chromoblastomycosis
Chromoblastomycosis can sometimes be confused with other skin conditions that may include:
- Squamous cell carcinoma
- Skin disorders such as discoid lupus erythematosus, psoriasis
- fungal infections that may consist of sporotrichosis
- Bacterial diseases such as tuberculosis, atypical mycobacterium infection, syphilis, and leprosy
- Protozoal infections like leishmaniasis
Diagnosis
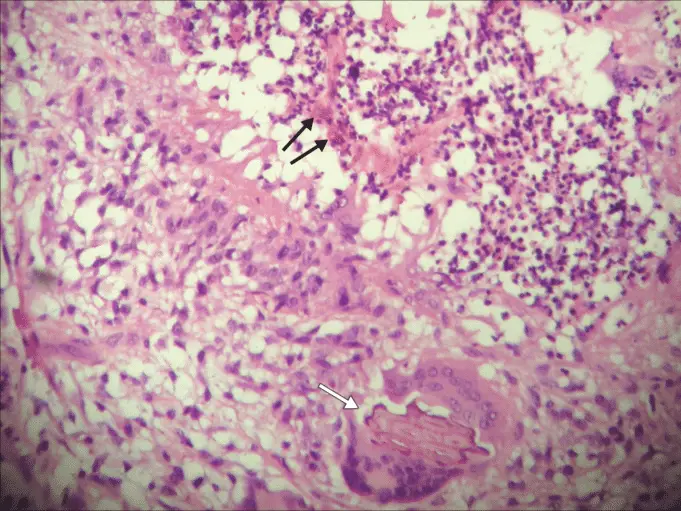
Histopathology of the infection may display typical thick-walled dark-brown ‘sclerotic’ cells on skin biopsy supporting the presence of dematiaceous fungus.
It is dark coloured due to melanin in the walls of the organism. Your medical doctor would have to add potassium hydroxide to the scaped lesion, then have it examined under a microscope.
Scrapings can be cultured to help with identifying the organism that is responsible. Specific strains, such as Gömöri methenamine silver and periodic acid Schiff, can help to demonstrate the fungal organisms when necessary.
Prevention
There are currently no means of preventing chromoblastomycosis apart from avoiding the traumatic fungal infection. Walking barefoot in endemic parts increases the chances of contracting the infection.
Treatment
Occasionally, chromoblastomycosis resolves naturally but would leave a scar. While treatment may be prolonged and a bit complicated, the primary treatment options may include:
- Local heat
- Flucytosine
- Thiabendazole
- Cryotherapy
- Itraconazole, voriconazole, or posaconazole and probably in combination with terbinafine
- Surgery to extract affected tissue
Bacterial superinfections can also be treated with the use of antibiotics.
Sources;