Benign paroxysmal positional vertigo (BPPV) is a condition that arises from a problem in the inner ear. BPPV induces short episodes of mild to intense dizziness.
It is usually caused by specific changes in the position of the head. This may happen when you tip your head up or down, lie down, or turn over or sit in bed.
BPPV may result from a head injury or may simply occur among older adults. A specific cause is often not identified. The underlying mechanism involves a small calcified otolith moving loosely in the inner ear.
It is a type of balance disorder with labyrinthitis and Ménière ‘s disease. Diagnosis is typically performed when the Dix – Hallpike test results in nystagmus (specific eye movement pattern) and other possible causes have been ruled out. In typical cases, medical imaging is not required.
Although BPPV can be frustrating and infuriating, it is rarely severe except when it raises the chance of falling. One may receive adequate treatment for BPPV during a visit to the doctor’s office.
The symptoms are replicated, brief periods of dizziness with movement, that is, of a spinning sensation after alteration in the position of the head. This can happen when you turn in bed or change position.
Each vertigo episode usually lasts less than a minute. Nausea is commonly associated with it. In this condition, dizziness is typically largely attributed to debris accumulated within the inner ear.
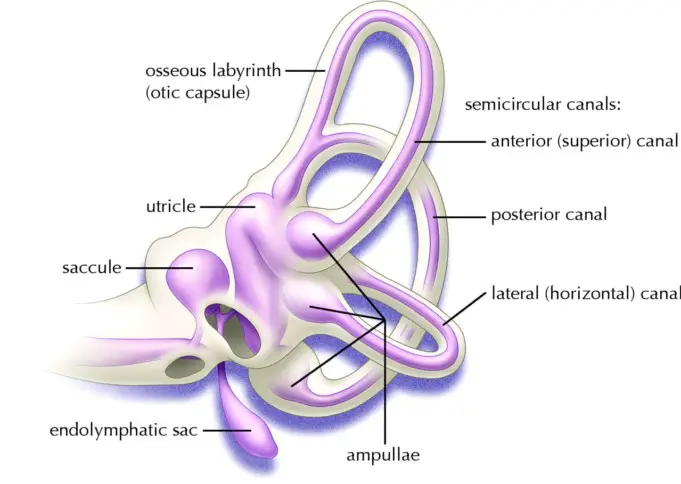
This debris can be referred to as “ear rocks,” even though the formally called “otoconia.” Ear rocks are small calcium carbonate crystals derived from the structure of the ear called the “utricle.”
While the saccule also contains otoconia, it is not capable of moving to the canal system. The utricle could have been damaged by head injury, infection, or other inner ear disorder, or could have deteriorated due to advanced age.
BPPV is the prevalent cause of dizziness. On average, about 1.6 per cent of the population has BPPV every year, of which about 0.6 per cent started that year. Approximately 20% of all dizziness seen in medical facilities is caused by BPPV.
BPPV may occur in children but is rare. BPPV is much more common in older people. Approximately 50 per cent of all dizziness in older people is due to BPPV. In one study, 9 per cent of urban dwelling elders were found to have non-diagnosed BPPV.
The symptoms of BPPV include vertigo or dizziness, nausea, lightheadedness, and imbalance. Activities which bring on symptoms will vary from person to person, but signs are almost always triggered by a change of the head position.
Getting out of bed early in the morning or rolling over in bed while asleep are common motions problems. People with BPPV usually feel dizzy and imbalanced when they tip their heads back to look up.
Women with BPPV can find that the use of shampoo bowls in beauty saloons brings on symptoms. Some Yoga postures or Pilates positions are triggers. BPPV could be present for a few weeks, then stop, then reoccur again.
Causes of Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is mainly discovered in ageing persons, and in older people, the most prevalent cause of degeneration or wear and tear of the vestibular system of the inner ear involves otoliths. In cases like this, BPPV is called “idiopathic”.
Head injuries are the most prevalent cause of BPPV in people under the age of 50. Head injury does not have to be that direct-even whiplash injuries have a significant incidence of BPPV. Between 8% and 20% of BPPV is linked to trauma.
There is also a significant correlation between BPPV and migraine. Viruses that affect the ear, such as those that cause vestibular neuritis and Meniere’s disease, are significant causes.
Although the toxicity of gentamicin is rarely found, BPPV is common in people who have been treated with ototoxic drugs such as gentamicin.
Diagnosis of BPPV
A physician can make the diagnosis relying on findings on physical examination, history and vestibular and auditory tests. Although, the diagnosis can be made with history and physical examination alone.
An example of a physical exam is Dix-Hallpike, In this test, a person is brought from sitting to lying horizontally with the face and torso facing up, with the head rotated 45 degrees to one side and rotated about 20 degrees backward.
Tests for BPPV can be made more accurate by making the patient wear video or Frenzel goggles. Most doctors or physical therapists that specialize in seeing dizzy patients usually keep a pair of those in their office.
A magnetic resonance imaging (MRI) scan can be carried out if a brain tumour or stroke is suspected. A rotatory chair test can be used for difficult diagnostic problems. It is possible, although rare to have BPPV in both ears (bilateral BPPV).
Electronystagmography (ENG) testing might be needed to look for the characteristic nystagmus (jumping of the eyes) induced by the Dix-Hallpike test. For the diagnosis of BPPV with laboratory tests, it is essential to have the ENG test done by a suitable laboratory so they can measure vertical eye movements.
Treatment
BPPV can often bee described as “self-limiting” because symptoms often subside or disappear within 1-2 months of onset. BPPV is usually not life-threatening. So one can decide to wait it out.
If one decides to wait, one may need to make some changes to one’s daily activities to cope with your dizziness. Use two or more pillows in the night. Avoid sleeping on the “bad” side of the house.
In the morning, one should stand up slowly and sit on the bed for 60 seconds. They should avoid bending down to pick up things, or stretching one’s head while getting something out of a cabinet.
They have to be careful when at the dentist’s office, and when getting one’s hair washed, or participating in sports activities, and when lying flat on one’s back. In the same way, they should be careful with chiropractic treatments that can jostle the head.
Symptoms tend to fade and wane. Motion sickness medications are sometimes beneficial in controlling nausea associated with BPPV but are otherwise rarely helpful.
These are two BPPV treatments that are usually undertaken in the doctor’s office. Both treatments are indeed very effective, with a cure rate of approximately 80%.
The two treatment are named after their inventors. Epley and Semont manoeuvres are both intended to transfer dirt or “ear rocks” out of the affected part of the ear to a not affected part of the ear. Each manoeuvre takes 15 minutes to achieve.
The Semont manoeuvre, also known as the Liberation manoeuvre, entails a procedure in which the patient moves quickly from lying on one side to lying on the other.
It is a fast-paced activity that is not currently practised in the United States, however, are 90% effective after four treatment sessions. This is similar to the Epley manoeuvres. Because the positions of the head are identical, the results are the same.
The Epley maneuver was invented by Dr John Epley. It is also called the particle repositioning or canalith repositioning procedure. It involves the concurrent movement of the head to four positions, remaining in each position for approximately 30 seconds.
It usually begins with the bad ear down. The recurrence rate for BPPV after these manoeuvres and resolution is about 22 per cent for one year and a second (or more) treatment may be required.
There is also a manoeuvre known as the “Foster manoeuvre,” which involves moving the head forward instead of backward, like in Semont and Epley. This manoeuvre may also be used to obtain similar results to those of Semont and Epley. We think this is a bit more difficult to pull out than the Epley.
Caution should be recommended when performing the Epley exercise if neurological symptoms (e.g. weakness, numbness, visual changes other than vertigo) occur.
But sometimes, such symptoms are caused by the contraction of the vertebral arteries, and a stroke may happen if one continues for an extended period of time.
If the exercises are conducted without medical supervision, it is advisable to stop the exercises and consult the doctor.
If the exercises are monitored, given that the diagnosis of BPPV is well established, in most cases the manoeuvre is modified so that the positions are reached by body movements rather than by head movements.
After either one of those manoeuvres, one should be ready to follow the guidelines below, which are designed to lessen the possibility that debris might fall back into the part of the ear that is sensitive.
Instructions for Patients After Treatments
- Rest for 10 minutes after the manoeuvre is conducted before going home. This is to avoid brief bursts of dizziness pr quick spins as debris repositions themselves immediately after the manoeuvre. One is advised not to drive themselves home.
- Semi-recumbent sleep for the next night. This means sleeping with the head at a 45-degree angle that is halfway between being flat and upright. This can be achieved by using a reclining chair or by using pillows arranged on a couch. One is not permitted to go to a hairdresser or dentist for a day.
- For at least seven days it is advisable to avoid provoking head positions that might induce BPPV, to use two pillows when sleeping, to avoid sleeping on the affected ear and to not turn your head far down or far up.
- Be careful to avoid a head-extended position where you are lying on your back, especially with your head turned towards the affected side. This means being mindful in the beauty parlour, the dentist’s office, and while undergoing minor surgery. Please remember to remain as upright as doable. Low-back workouts should be stopped for one week. No “sit-ups” should be done for a week and no “crawl” swimming except Breaststroke. Also, avoid far forward positions such as those that may take place during specific exercises, e.g. touching your toes.
- Seven days after treatment, put yourself in the position that usually induces vertigo. Position yourself carefully and under conditions in which one can’t fall or hurt yourself. Let your doctor know-how about it.
Surgical treatment of Benign Paroxysmal Positional Vertigo
The amounts of surgical treatment for BPPV has been dropping rapidly in favour of other modes of treatments. Only one in 200 BPPV patients eventually do this procedure.
Surgery should only be considered when all three manoeuvres/exercises have been attempted and didnt work.
Indications for surgery
If the exercises inefficient in controlling symptoms, symptoms continue for a year or longer, and the diagnosis is very evident, a surgical procedure called “posterior canal plugging” may be advised.
Canal plugging blocks most of the function of the posterior canal without posing a risk to parts of the ear. This procedure poses a significant hearing risk, ranging from 3-20 per cent, but is useful in approximately 85-90 per cent of individuals who have not responded to any other treatment.
The risk of hearing surgery arises from the inadvertent rupture of the endolymphatic compartment while attempting to open the bone labyrinth with a drill. However, this mode of treatment is rarely undertaken due to the risk to hearing.
Lifestyle and home remedies
BPPV can recur after successful therapy. Even though there’s no cure, it can be managed effectively with physical therapy and home treatments.
If you suffer from dizziness caused by BPPV, consider these tips:
- Always remember you can lose your balance, which can result to falling or serious injury.
- Avoid abrupt movements, such as looking up, that can induce symptoms.
- Sit down or find a place to lean on dizzy.
- Use appriopriate lighting at night.
- Walk with a cane for support if you’re at risk of falling.
- Consult with your doctor regularly to manage your symptoms.
Preparing for your appointment
Schedule your appointment with the doctor if you have symptoms common to BPPV. The doctor will carry out an examination, and may refer you to an ear, nose and throat (ENT) specialist or neurologist.
Here’s some information to help you get ready for your appointment.
- Write down the symptoms you are experiencing, including when they began and how frequently they occur.
- Write down any recent injuries to your head, including even minor accidents.
- Make a list of your preexisting medical information, this dhould include any for which you’re being treated and the names of any medications, supplements and vitamins you’re taking.
- Write down questions you would like to as the doctor. Making your list of questions can help you maximize the most of your time.
Questions to ask the doctor at the initial appointment include:
- What are the likely causes of my symptoms?
- What tests do are they recommending?
- Are there any activities i should avoid while waiting for a diagnosis?
- Do I need to see a specialist?
What to expect from your doctor
A doctor who sees you for symptoms associated with BPPV may ask some questions, such as:
- What are your symptoms, and when did they start?
- Do your symptoms come and go? How often?
- How long do your symptoms last?
- Does anything, in particular, seem to trigger your symptoms, such as certain types of movement or activity?
- Do your symptoms include vision problems?
- Do your symptoms include nausea or vomiting?
- Do your symptoms include headache?
- Have you lost any hearing?
- Are you being treated for any other medical conditions?
References;
- Benign paroxysmal positional vertigo (BPPV); Mayo Clinic, Wikipedia